I think I've found a pretty good remedy for the retch factor that had been interfering with my strength-training workouts. The super shake lunch/afternoon snack really does seem to make quite a difference with respect to the problem I've been experiencing. So I'll be continuing to have a super shake for lunch/afternoon snack on strength-training days: it really seems to be about the best resolution to the problem that I'm going to find.
Having said that I have to point out that the problem is not completely alleviated by the super shake . . . for want of a better word . . . let's say, diet. When I'm pushing myself very hard I do still feel some back pressure from the stomach--especially when I'm doing some exercise that involves bending over. But the feeling is much less intense, and thus is less likely to interfere with my breathing pattern.
So, once again, if you, like me, have this problem of feeling as though you're going to regurgitate during intense exercise, try switching to a lighter meal like the super shake on your workout days. I make a really large one, of which I consume about three quarters for lunch. (at about 12:30 P.M.) I consume the other one quarter at about 3 P.M. as a snack and by the time our strength-training routine occurs (around 6 P.M.) I'm able to push hard with minimal interference from the retch factor.
The burning sensation I get in my chest when doing intervals, though, continues to plague me. I'll undoubtedly be writing further about that sensation and its connection with the retch factor in future entries. Stay tuned for those.
Sunday, January 31, 2010
Saturday, January 30, 2010
Madonna does menopause
So Madonna's been in the press in the not-too-distant past because of what's considered her extreme fitness undertakings. People are ogling at her biceps. Marveling at her endurance. They're spellbound by her dedication. Etc.
Well, guess what? Madonna's my age--less than 6 months my senior. She's doing fitness--the subject of my blog--so she's on-topic here, right?
I really can't tell you much about Madonna other than that she's a singer. I guess I missed the Madonna boat--along with the boats of a lot of other entertainment figures that post-date about 1980. I occassionally catch wind of some thing or other she's done but I'm not too enamored of pop culture so I sort of missed all the hubub. And so far as I can tell, I didn't miss much.
I have no idea what songs she's sung, though I vaguely remember a title like "Modern Girl" or something along those lines. Nope, no idea what the melody for that one is. The only melody of any song of hers I know is her remake of "Santa Baby," a song that became popular among the playboy/nightclub crowd in the 50's. I heard the song in the drugstore once and became curious about it so I looked it up online and found out she was the singer of this new version.
But anyway, I think I know what's going on with Madonna these days. It's called menopause. As is commonly understood, women undergoing menopause--like those undergoing the other big feminine hormonal change, puberty--can have odd reactions. There are hot flashes, mood swings, physiological changes. People around these women sometimes feel they've gone a little batty in the initial phases.
Well, here's my proposition: what happens when a woman whose life and business is her public persona and she has limitless funding to devote to those things, when she hits menopause? Might not Madonna's answer be to go on an extreme fitness binge, hire the best personal trainers, buy the best exercise equipment, and spend hours working out? I submit that the answer to that question is "yes."
I further submit that she's, well, gone a bit bonkers with it. But hey, that's what women do when they hit this point in their lives. I do think it's a good thing for women to do fitness, especially right around menopause, when they start to lose bone density. So I don't begrudge her working out. But I do think she's gone overboard with it and that this can be explained by the hormonal imbalance.
And no, I don't care of you think I'm sexist for saying that.
Well, guess what? Madonna's my age--less than 6 months my senior. She's doing fitness--the subject of my blog--so she's on-topic here, right?
I really can't tell you much about Madonna other than that she's a singer. I guess I missed the Madonna boat--along with the boats of a lot of other entertainment figures that post-date about 1980. I occassionally catch wind of some thing or other she's done but I'm not too enamored of pop culture so I sort of missed all the hubub. And so far as I can tell, I didn't miss much.
I have no idea what songs she's sung, though I vaguely remember a title like "Modern Girl" or something along those lines. Nope, no idea what the melody for that one is. The only melody of any song of hers I know is her remake of "Santa Baby," a song that became popular among the playboy/nightclub crowd in the 50's. I heard the song in the drugstore once and became curious about it so I looked it up online and found out she was the singer of this new version.
But anyway, I think I know what's going on with Madonna these days. It's called menopause. As is commonly understood, women undergoing menopause--like those undergoing the other big feminine hormonal change, puberty--can have odd reactions. There are hot flashes, mood swings, physiological changes. People around these women sometimes feel they've gone a little batty in the initial phases.
Well, here's my proposition: what happens when a woman whose life and business is her public persona and she has limitless funding to devote to those things, when she hits menopause? Might not Madonna's answer be to go on an extreme fitness binge, hire the best personal trainers, buy the best exercise equipment, and spend hours working out? I submit that the answer to that question is "yes."
I further submit that she's, well, gone a bit bonkers with it. But hey, that's what women do when they hit this point in their lives. I do think it's a good thing for women to do fitness, especially right around menopause, when they start to lose bone density. So I don't begrudge her working out. But I do think she's gone overboard with it and that this can be explained by the hormonal imbalance.
And no, I don't care of you think I'm sexist for saying that.
Friday, January 29, 2010
Gone in 60 seconds!
Ok, so the title of this entry is a bit cliche--but only for those of us old enough to remember when the cliche was current!1 For those who are not old enough, the following explanation.
This was the title of a suspense movie about car theft. The title intends to indicate how easy it was in that era (early 70's) to steal a car: it took only one minute for these thieves to make off with your car. I never saw the movie myself, but it was advertised heavily enough and I was at a sufficiently impressionable age that its title and theme got (unfortunately) burned into my psyche.
Well, in this entry, I'm using the cliche to refer to something quite unrelated to car thievery. Nonetheless the concept that title sought to encapsulate struck me as appropriate to what I'm blogging about today--insomnia . . . again.
You see, night before last was a zolpidem (aka Ambien) night. I'd decided prior to that night that I'd had enough restless nights in a row that I had to do something to get a decent night's sleep.
To expand a bit on something I relegated to a footnote in my blood pressure chart, I'd had a high blood pressure reading subsequent to one of the difficult nights I had this week and decided "ok, it's time to get a good night's sleep." So I took the zolpidem the other night with the expected results: slept solidly from about 11 PM to 4 AM (very rare occurrence). Got up for a bladder run and had a sensation as though all the intestinal distress that had been going on during those five hours was suddenly hitting me at that moment. But I nonetheless had no trouble getting back to sleep, finally arising only at a little before 8 AM.
What a refreshing feeling after so many fitful nights. I felt pretty good the whole day. And even going in to last night I felt fine, though I did have a bit of intestinal discomfort prior to retiring for the night.
But last night turned out to be another one of those pretty much sleepless nights. My body kept trying to fall asleep, but I kept jolting awake somehow. That went on from about 1 AM to 4 AM, during which time I probably dozed off and woke up at least a dozen times. By 4 AM I couldn't get even doze off anymore, but just lay there tossing and turning.2 So I got up.
I tried to rest again after breakfast but for me, as for probably most other people, it's difficult to sleep when it's daylight. So I got in maybe 2.5 hours of slightly less fitful sleep after breakfast. And here I am again, well on my way to another episode of sleep deficit.
Now is it clear why I've chosen the title I have for this entry? Yesterday I was on the road to feeling fine sleep-wise: today I'm on my way back to where I was before I took the zolpidem.3 Sleep adequacy . . . gone in (a little bit more than) 60 seconds.
------------------
1 Ok, call me a complete pop-culture neanderthal. I don't care. I discovered after writing this entry that a remake of this early 70's movie was done in 2000. So what?
2 This is actually the pattern for most nights when I do not take zolpidem.
3 In case your'e wondering why I don't take the zolpidem more regularly, take a look here.
This was the title of a suspense movie about car theft. The title intends to indicate how easy it was in that era (early 70's) to steal a car: it took only one minute for these thieves to make off with your car. I never saw the movie myself, but it was advertised heavily enough and I was at a sufficiently impressionable age that its title and theme got (unfortunately) burned into my psyche.
Well, in this entry, I'm using the cliche to refer to something quite unrelated to car thievery. Nonetheless the concept that title sought to encapsulate struck me as appropriate to what I'm blogging about today--insomnia . . . again.
You see, night before last was a zolpidem (aka Ambien) night. I'd decided prior to that night that I'd had enough restless nights in a row that I had to do something to get a decent night's sleep.
To expand a bit on something I relegated to a footnote in my blood pressure chart, I'd had a high blood pressure reading subsequent to one of the difficult nights I had this week and decided "ok, it's time to get a good night's sleep." So I took the zolpidem the other night with the expected results: slept solidly from about 11 PM to 4 AM (very rare occurrence). Got up for a bladder run and had a sensation as though all the intestinal distress that had been going on during those five hours was suddenly hitting me at that moment. But I nonetheless had no trouble getting back to sleep, finally arising only at a little before 8 AM.
What a refreshing feeling after so many fitful nights. I felt pretty good the whole day. And even going in to last night I felt fine, though I did have a bit of intestinal discomfort prior to retiring for the night.
But last night turned out to be another one of those pretty much sleepless nights. My body kept trying to fall asleep, but I kept jolting awake somehow. That went on from about 1 AM to 4 AM, during which time I probably dozed off and woke up at least a dozen times. By 4 AM I couldn't get even doze off anymore, but just lay there tossing and turning.2 So I got up.
I tried to rest again after breakfast but for me, as for probably most other people, it's difficult to sleep when it's daylight. So I got in maybe 2.5 hours of slightly less fitful sleep after breakfast. And here I am again, well on my way to another episode of sleep deficit.
Now is it clear why I've chosen the title I have for this entry? Yesterday I was on the road to feeling fine sleep-wise: today I'm on my way back to where I was before I took the zolpidem.3 Sleep adequacy . . . gone in (a little bit more than) 60 seconds.
------------------
1 Ok, call me a complete pop-culture neanderthal. I don't care. I discovered after writing this entry that a remake of this early 70's movie was done in 2000. So what?
2 This is actually the pattern for most nights when I do not take zolpidem.
3 In case your'e wondering why I don't take the zolpidem more regularly, take a look here.
Wednesday, January 27, 2010
Seafood, y'all?
"And now," as they used to say on Monty Python, "for something completely different . . ."

Ok, so it's got nothing to do with fitness after 50 and is only marginally related to (unhealthy) diet. But it was just too funny to pass up. Hot dogs, Kraft instant macaroni and canned green beans--yum! Don't you think those squid dogs would look a lot cuter if they'd carved little smiles in them, too? And you can rest assured those aren't tofu dogs (I found this photo while searching google images for pictures of seafood, incidentally).
More substantial entries will be forthcoming. I got my new interval timer, so I can review that soon. Then, I've still got a more detailed creatine report to give.
Redneck Seafood dinner

Ok, so it's got nothing to do with fitness after 50 and is only marginally related to (unhealthy) diet. But it was just too funny to pass up. Hot dogs, Kraft instant macaroni and canned green beans--yum! Don't you think those squid dogs would look a lot cuter if they'd carved little smiles in them, too? And you can rest assured those aren't tofu dogs (I found this photo while searching google images for pictures of seafood, incidentally).
More substantial entries will be forthcoming. I got my new interval timer, so I can review that soon. Then, I've still got a more detailed creatine report to give.
Tuesday, January 26, 2010
Resistance training improves mental function in the elderly
In this entry I'll present material from a recently-published study1 that offers compelling evidence that resistance training can improve mental function as we age. I'd be a bit young to qualify for a study like this--plus I'm the wrong gender (it was an all-woman test group)--but the results are nonetheless heartening to those of us drawing closer to the ages of the participants (65-75).
Here are some salient--though somewhat technical--excerpts:
Actually, on that note, the authors mention the following: "intervention studies have shown that aerobic exercise training enhances brain and cognitive function." So it seems it's already been established that aerobic exercise enhances brain function in older subjects: this study's aim, on the other hand, was to see whether the same or similar benefits would come from resistance training.
So the ladies doing the resistance training made notable improvements in one area of mental function--what the authors call "enhanced selective attention and conflict resolution"--though not in other areas. Interestingly, the authors mention a similar study done with male participants that showed improvements in other areas of brain function:
-----------------------
1 Arch Intern Med. 2010;170(2):170-178
Here are some salient--though somewhat technical--excerpts:
Resistance Training and Executive Functions A 12-Month Randomized Controlled TrialOk, so they divided this group of ladies into two sub-groups and had each perform a type of exercises. One type of exercise was resistance training--what I would call strength training--while the other group did balance and toning exercises. What, exactly, were the exercises they were doing? Further on, the article indicates the following:
Teresa Liu-Ambrose, PhD, PT; Lindsay S. Nagamatsu, MA; Peter Graf, PhD;
B. Lynn Beattie, MD; Maureen C. Ashe, PhD, PT; Todd C. Handy, PhD
Background: Cognitive decline among seniors is a pressing health care issue. Specific exercise training may combat cognitive decline. We compared the effect of once-weekly and twice-weekly resistance training with that of twice-weekly balance and tone exercise training on the performance of executive cognitive functions in senior women.
Methods: In this single-blinded randomized trial, 155 community-dwelling women aged 65 to 75 years living in Vancouver were randomly allocated to once-weekly (n = 54) or twice-weekly (n = 52) resistance training or twice-weekly balance and tone training (control group) (n = 49). The primary outcome measure was performance on the Stroop test, an executive cognitive test of selective attention and conflict resolution. Secondary outcomes of executive cognitive functions included set shifting as measured by the Trail Making Tests (parts A and B) and working memory as assessed by verbal digit span forward and backward tests. Gait speed, muscular function, and whole-brain volume were also secondary outcome measures.
Results: Both resistance training groups significantly improved their performance on the Stroop test compared with those in the balance and tone group (P .03). Task performance improved by 12.6% and 10.9% in the once-weekly and twice-weekly resistance training groups, respectively; it deteriorated by 0.5% in the balance and tone group. Enhanced selective attention and conflict resolution was significantly associated with increased gait speed. Both resistance training groups demonstrated reductions in whole-brain volume compared with the balance and tone group at the end of the study (P .03).
Conclusion: Twelve months of once-weekly or twice-weekly resistance training benefited the executive cognitive function of selective attention and conflict resolution among senior women.
Resistance TrainingGlad they didn't mention tandem riding under the Balance and Tone category . . .
The resistance training program used a progressive, high-intensity protocol. The air-pressured digital resistance leg press machine and free weights were used to provide the training stimulus. The leg press machine based exercises consisted of biceps curls, triceps extension, seated rowing, latissimus dorsi pull-down exercises, leg presses, hamstring curls, and calf raises. The intensity of the training stimulus was at a work range of 6 to 8 repetitions (2 sets). The training stimulus was subsequently increased using the 7-RM method, when 2 sets of 6 to 8 repetitions were completed with proper form and without discomfort. Other key strength exercises included minisquats, mini-lunges, and lunge walks. The number of sets completed and the load lifted for each exercise were recorded for each participant at every class.
Balance and Tone
The balance and tone program consisted of stretching exercises, range-of-motion exercises, basic core-strength exercises including kegels (ie, exercises to strengthen the pelvic floor muscles), balance exercises, and relaxation techniques. Key balance exercises included tai chibased forms (ie, the crane and the tree pose), tandem stand, tandem walking, and single leg stance (eyes opened and closed). Other than body weight, no additional loading (eg, hand weights or resistance bands) was applied to any of the exercises. There is no evidence that these exercises improve cognitive function. This group served to control for confounding variables such as physical training received by traveling to the training centers, social interaction, and changes in lifestyle secondary to study participation.
Actually, on that note, the authors mention the following: "intervention studies have shown that aerobic exercise training enhances brain and cognitive function." So it seems it's already been established that aerobic exercise enhances brain function in older subjects: this study's aim, on the other hand, was to see whether the same or similar benefits would come from resistance training.
So the ladies doing the resistance training made notable improvements in one area of mental function--what the authors call "enhanced selective attention and conflict resolution"--though not in other areas. Interestingly, the authors mention a similar study done with male participants that showed improvements in other areas of brain function:
Cassilhas et al demonstrated that 6 months of thrice-weekly moderate- or high-intensity resistance training improved cognitive performance of memory and verbal concept formation among senior men. Our findings extend these results in several critical ways. Most notably, our results suggest that the effects of resistance training on executive cognitive functions appear to be selective; that is, resistance training enhanced selective attention and conflict resolution in older women, but cognitive abilities associated with manipulating verbal information in working memory and shifting between task sets or instructions were not improved.Still, the net result of the study seems to be that, as we age, brain and cognitive function can be enhanced by exercise--whether of the strength- or resistance-training, or of the aerobic sort--or both.
-----------------------
1 Arch Intern Med. 2010;170(2):170-178
Monday, January 25, 2010
Diet musings
In addition to the reading and research I do as I maintain and enhance this blog, I've taken to consulting a few fitness blogs lately. I've bumped into a fair amount of discussion of diets on these blogs, and generally I find this discussion a little frustrating. I'll explain why in this entry.
To me it's frustrating because, while I'm interested in maintaining a healthy diet and reading about nutrition, these discussions inevitably turn to weight loss questions and debate about how well or poorly this or that diet reduce fat. I can understand in a certain respect why this is the case: diets, as we all know, are most often formulated for and followed by, those who are obese or otherwise unhealthy.
For me, the discussion becomes frustrating at this point because I don't need to lose any weight. Plus, I already eat a fairly healthy diet (long-time pesco-vegetarian, don't eat fast food with any regularity, love fruits, vegetables, and whole grains). So when these dietary discussions start to turn to weight loss--as they invariably do--I feel that my attempts at gleaning useful information are being subverted: I just want to know how foods might benefit or harm an already healthy body, not how they might make me lose weight.
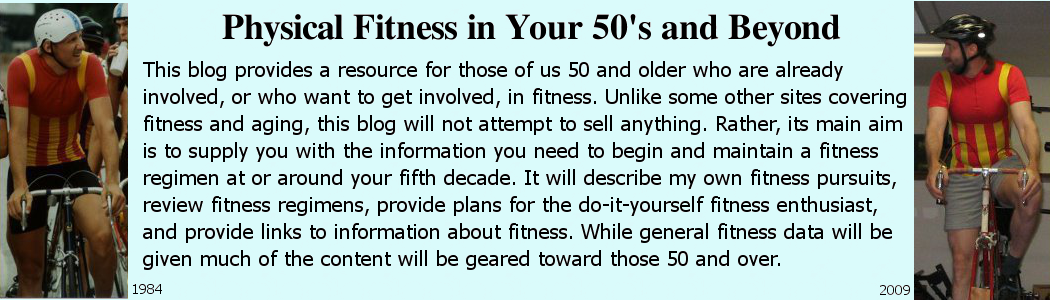
For the sake of furthering this discussion, a few more words about myself. I have no idea what my bodyfat percentage is, but I know it's on the low side. I have a pretty athletic build--as you might gather from the photos in the heading of this blog. I am a little thicker around the mid-section in the 2009 photo than in the 1984 photo, so I definitely have more bodyfat now than I did then (is it 2, 3, maybe 4 percentage points?). But comparatively (to other 50-year-old males), I nonetheless now have pretty low bodyfat.
Could my bodyfat be lower? Undoubtedly it could. I doubt getting it lower would improve my overall health, but I could certainly lower it further. So far as I can tell the impetus for doing that would probably be vanity rather than health. And thus far I've found that, during cycling season when we're putting in plenty of long, hard rides, I do shed about 5 lbs. and get down around 200, give or take a pound or two. So I do see some seasonal variation in weight and thus, I would guess, variation in bodyfat.
Getting back to the dietary material I've been reading. I'm left in a state of confusion about it. My weight is pretty good and I don't see a significant health gain in lowering my bodyfat any further. Moreover my most recent cholestrol readings approach magnificence (see my "vital stats" for those). So does that mean my diet is fine? Should I just ignore all this dietary information I'm finding, or are there things I need to change about my diet? Perhaps I should leave well enough alone?
Is there any source that aims to help people who are already fairly trim and not eating a lot of trash food, adjust their diets? I'm still looking . . .
To me it's frustrating because, while I'm interested in maintaining a healthy diet and reading about nutrition, these discussions inevitably turn to weight loss questions and debate about how well or poorly this or that diet reduce fat. I can understand in a certain respect why this is the case: diets, as we all know, are most often formulated for and followed by, those who are obese or otherwise unhealthy.
For me, the discussion becomes frustrating at this point because I don't need to lose any weight. Plus, I already eat a fairly healthy diet (long-time pesco-vegetarian, don't eat fast food with any regularity, love fruits, vegetables, and whole grains). So when these dietary discussions start to turn to weight loss--as they invariably do--I feel that my attempts at gleaning useful information are being subverted: I just want to know how foods might benefit or harm an already healthy body, not how they might make me lose weight.
For the sake of furthering this discussion, a few more words about myself. I have no idea what my bodyfat percentage is, but I know it's on the low side. I have a pretty athletic build--as you might gather from the photos in the heading of this blog. I am a little thicker around the mid-section in the 2009 photo than in the 1984 photo, so I definitely have more bodyfat now than I did then (is it 2, 3, maybe 4 percentage points?). But comparatively (to other 50-year-old males), I nonetheless now have pretty low bodyfat.
Could my bodyfat be lower? Undoubtedly it could. I doubt getting it lower would improve my overall health, but I could certainly lower it further. So far as I can tell the impetus for doing that would probably be vanity rather than health. And thus far I've found that, during cycling season when we're putting in plenty of long, hard rides, I do shed about 5 lbs. and get down around 200, give or take a pound or two. So I do see some seasonal variation in weight and thus, I would guess, variation in bodyfat.
Getting back to the dietary material I've been reading. I'm left in a state of confusion about it. My weight is pretty good and I don't see a significant health gain in lowering my bodyfat any further. Moreover my most recent cholestrol readings approach magnificence (see my "vital stats" for those). So does that mean my diet is fine? Should I just ignore all this dietary information I'm finding, or are there things I need to change about my diet? Perhaps I should leave well enough alone?
Is there any source that aims to help people who are already fairly trim and not eating a lot of trash food, adjust their diets? I'm still looking . . .
Sunday, January 24, 2010
Short note on intervals
Intervals continue to go well. The time seems to go by so much more quickly when you're keeping track of time in 3.5-minute increments. We're averaging about 20-25 minutes per interval session. We do about 6 intervals in total, which amounts to about 3.5 minutes of intense exercise interspersed with about 20 minutes of light-duty aerobics.
I've gone ahead an ordered an interval timer to aid us in executing these. Intervals will for sure remain an integral part of our off-season bicycle training.
I should have another creatine update tomorrow after we've done another strength-training session.
I've gone ahead an ordered an interval timer to aid us in executing these. Intervals will for sure remain an integral part of our off-season bicycle training.
I should have another creatine update tomorrow after we've done another strength-training session.
Saturday, January 23, 2010
Another installment on super shakes and creatine
Ok, now that I've done a handful of strength-training workouts after starting creatine I have some more data to report. Also, I started having a super shake for lunch/afternoon snack on strength-training days as a means of possibly counteracting what I called the "retch factor," so I have information to report on how that's gone as well. Would've posted this last night, but this Saturday was a really busy one that also took up part of Friday.
First, about the super shake remedy for retch factor. As you'll recall, I was having a problem pushing myself in strength-training workouts because of the retch factor, which necessitated suppressing the urge to, well, vomit. I came up with the idea of, instead of eating solid food on strength-training days, having more of a liquid lunch to see whether that might mitigate or eliminate the retch factor.
So we've now done two strength-training workouts on days when I had a super shake for lunch--actually an extra large one that I even save a portion of for a mid-afternoon snack. And I have to say that having this sort of lunch does definitely mitigate the retch factor.
I can't say that, on days so far when I've tried the super-shake lunch, I don't feel any sort of regurgitative urges whatsoever while pushing myself hard during strength training. But I can say that I feel that much less frequently and urgently, and can consequently push myself harder. So I'm sticking with this diet for strength-training days. If you have a similar problem with the retch factor, I recommend you also try the super shake remedy. I'm glad I tried this.
I also have to report, on a related note, that I've been experiencing this intense burning in the chest, and that I identified with the retch factor, during our recent interval training sessions. And I'm beginning to think that the burning sensation, while often accompanied by the urge to regurgitate, may actually be a separate sensation.
I cannot say, for example, that during our recent strength-training sessions when I got that regurgitative urge, it was accompanied by burning in the chest: sometimes it is, sometimes not. I'm still working on analyzing the interrelation of the two and will likely post more on this topic later.
Finally, I have kind of a mixed review of creatine. During Monday's workout I definitely felt the effects of the creatine. I felt as though I was able to use heavier weights and that I didn't get nearly as winded as I had been. I was ready, at that point, to pretty much reverse initial observations I'd made about creatine. But then came Friday's workout.
During Friday's strength-training workout, I can't say I felt much of anything at all from the creatine. Perhaps a slight decrease in recovery time, but nothing nearly as dramatic as I felt on Monday. So I have to say it's still a bit of a mixed bag on the creatine front. I'll need more time to assess the situation. That said, I do feel some slight mental benefits from it.
As for why the creatine seemed to have a much more dramatic effect on Monday than on Friday, one possibility is that Monday was much closer to the end of the creatine "loading phase," so I likely had more of it in my system at that point than on Friday. Also, I actually reduced the dosage during the course of this week from the recommended full teaspoon to half a teaspoon. So I will try increasing it back to the normal dosage and see what effect that has on next week's strength-training workouts.
Look for further reports later.
First, about the super shake remedy for retch factor. As you'll recall, I was having a problem pushing myself in strength-training workouts because of the retch factor, which necessitated suppressing the urge to, well, vomit. I came up with the idea of, instead of eating solid food on strength-training days, having more of a liquid lunch to see whether that might mitigate or eliminate the retch factor.
So we've now done two strength-training workouts on days when I had a super shake for lunch--actually an extra large one that I even save a portion of for a mid-afternoon snack. And I have to say that having this sort of lunch does definitely mitigate the retch factor.
I can't say that, on days so far when I've tried the super-shake lunch, I don't feel any sort of regurgitative urges whatsoever while pushing myself hard during strength training. But I can say that I feel that much less frequently and urgently, and can consequently push myself harder. So I'm sticking with this diet for strength-training days. If you have a similar problem with the retch factor, I recommend you also try the super shake remedy. I'm glad I tried this.
I also have to report, on a related note, that I've been experiencing this intense burning in the chest, and that I identified with the retch factor, during our recent interval training sessions. And I'm beginning to think that the burning sensation, while often accompanied by the urge to regurgitate, may actually be a separate sensation.
I cannot say, for example, that during our recent strength-training sessions when I got that regurgitative urge, it was accompanied by burning in the chest: sometimes it is, sometimes not. I'm still working on analyzing the interrelation of the two and will likely post more on this topic later.
Finally, I have kind of a mixed review of creatine. During Monday's workout I definitely felt the effects of the creatine. I felt as though I was able to use heavier weights and that I didn't get nearly as winded as I had been. I was ready, at that point, to pretty much reverse initial observations I'd made about creatine. But then came Friday's workout.
During Friday's strength-training workout, I can't say I felt much of anything at all from the creatine. Perhaps a slight decrease in recovery time, but nothing nearly as dramatic as I felt on Monday. So I have to say it's still a bit of a mixed bag on the creatine front. I'll need more time to assess the situation. That said, I do feel some slight mental benefits from it.
As for why the creatine seemed to have a much more dramatic effect on Monday than on Friday, one possibility is that Monday was much closer to the end of the creatine "loading phase," so I likely had more of it in my system at that point than on Friday. Also, I actually reduced the dosage during the course of this week from the recommended full teaspoon to half a teaspoon. So I will try increasing it back to the normal dosage and see what effect that has on next week's strength-training workouts.
Look for further reports later.
Thursday, January 21, 2010
Alternative/natural sleep aids
I've blogged previously about the insomnia I've experienced over the last decade or so and about the fact that I suspect it may play a role in my heightened blood pressure. And thus may also be related to my current fitness endeavors, which were undertaken, in part, in reaction to high blood pressure readings. I've also blogged about how a medication I was prescribed--zolpidem (Ambien)--though it gave some relief from the insomnia, nevertheless caused me some serious mood problems when used with regularity.
Well, I cut back on using the zolpidem, though I am still experimenting with it. It does seem that, if I use it as seldom as once per week, the mood problems are either very minimal or absent. I'll now experiment with using it for two days in a given week to see if those same results hold. The aim is, of course, to figure out the proper dosage and scheduling: at what point does it give the undesirable side-effects and within what parameters do those side-effects not manifest to a problematic degree?
I'm finding that out. And I'll be reporting the results here.1
While performing those experiments, I've also considered the natural alternative sleep aids. My first option--were it legal or if I could legitimately obtain it--would be marijuana. I haven't used any for decades but, according to experiences I had with it in my youth, I would presume it could make a pretty effective sleep aid. But it's just not a realistic option given the current state of affairs in this country: I'd have to get involved with the underworld culture to try this and run the risk of falling afoul of the law. I'm just not interested--either in having those kinds of ties anymore or in confronting the justice system.
Another possible natural sleep aid I've read about recently is kava kava. That one can be legally obtained and I do hope to try it soon so as to see whether it can offer me an alternative to the zolpidem. So, look for future posts on the viability of using kava as a sleep aid.
----------------------------
1 Today's (1/22/10) results are encouraging. Having taken zolpidem for the second time within one week, I nonetheless can say that I do not feel any particular mood issues. I'm encouraged and plan to keep taking zolpidem up to 2 times per week to see if these preliminary positive results persist.
Well, I cut back on using the zolpidem, though I am still experimenting with it. It does seem that, if I use it as seldom as once per week, the mood problems are either very minimal or absent. I'll now experiment with using it for two days in a given week to see if those same results hold. The aim is, of course, to figure out the proper dosage and scheduling: at what point does it give the undesirable side-effects and within what parameters do those side-effects not manifest to a problematic degree?
I'm finding that out. And I'll be reporting the results here.1
While performing those experiments, I've also considered the natural alternative sleep aids. My first option--were it legal or if I could legitimately obtain it--would be marijuana. I haven't used any for decades but, according to experiences I had with it in my youth, I would presume it could make a pretty effective sleep aid. But it's just not a realistic option given the current state of affairs in this country: I'd have to get involved with the underworld culture to try this and run the risk of falling afoul of the law. I'm just not interested--either in having those kinds of ties anymore or in confronting the justice system.
Another possible natural sleep aid I've read about recently is kava kava. That one can be legally obtained and I do hope to try it soon so as to see whether it can offer me an alternative to the zolpidem. So, look for future posts on the viability of using kava as a sleep aid.
----------------------------
1 Today's (1/22/10) results are encouraging. Having taken zolpidem for the second time within one week, I nonetheless can say that I do not feel any particular mood issues. I'm encouraged and plan to keep taking zolpidem up to 2 times per week to see if these preliminary positive results persist.
Wednesday, January 20, 2010
The untold story: abdominal and other secret workouts I've not divulged here
I've got some post-preliminary reports (since I've already given a preliminary report) on creatine and super shakes, but I'll hold off on giving those until after this coming Friday's strength-training workout--so as to compile a bit more data. Meantime, I'll fill in with the current entry.
The title pretty much says it all: have I told you everything we do in the way of fitness? No, not everything. I've focused on the major components of our fitness regimen, i.e., the cycling/stationary-bike stuff for aerobic and lower-body strengthening on the one hand, and the strength-training workouts we do for upper body on the other. But there are actually a couple of other fitness routines that we work in, one of which I've not mentioned at all (shame on me).
The one I have mentioned is walking. We do sometimes replace cycling/stationary-bike riding with walking (2 - 8 miles)--as I've pointed out in a previous entry. But what I haven't mentioned is that I additionally try to walk about 1.5 miles on days when we have our strength training (Mon. and Fri.) and also on our rest day (Wed.). It's not much, but with age and being involved in an otherwise sedentary field of work, it's good to get in any extra activity you can. So there's that.
But what I've not mentioned at all is our abdominal workouts. We actually go fairly light on these, spending 5 minutes or so on cycling days performing them. One set of exercises that we do are ones that were given to me by a physical therapist who I was seeing last spring about some back pain. There are some crunches in there, an exercise called "dead bug," another called "mermaid," and another called "bird dog." These are as much core-strengthening exercises as abdominal exercises, though, of course, the two groups of muscles are closely related. Some of the movements remind me somewhat of Pilates exercises.
The other routine we do is one we appropriated from the Power 90 program. It's called "ab ripper 100." And our old friend Tony Horton leads the exercises.
Here's the list of exercises (10 moves, 10 reps each): 1 crunches, 2. left side crunch, 3. right side crunch, 4. elbows to knees, 5. superman crunch, 6. leg lifts, 7. in and outs, 8. hip rock, 9. bicycles, 10. full body crunch.
Using this routine has gone well for us so far--though I do sometimes hurt my back doing ab exercises: both the ab ripper routine and the other set of exercises I got from the physical therapist are liable to cause me lower-back trouble if I don't do them carefully. At the moment, in fact, we're taking a break from all abdominal exercises since I hurt my back about 10 days ago or so. But that hiatus should end soon. As will be evident from the time signature in these still frames, the whole routine only takes about 4.5 minutes
Anyway, I have thought of stepping up the abdominal workouts a bit during part of the year. Currently, I'm considering whether to replace our current abdominal routines with "ab ripper x" (jeez I hate these titles! I think I'll just call it "abdomen firmer" from now on) for part of the year. That's about a 15 minute routine, so it'd be quite a bit more intense than what we do now. But hey, I'm up for doing it for 2 or 3 months out of each year.
That's still in the planning stages, though. Look for further updates on the abdominal exercise front later. And by the way, don't I need to include these abdominal exercises at least somewhere in my overview of our regime? Another note to self: P90X's core synergistics DVD might be a good one to work into the abdominal/core regimen on occasion as well, no?
UPDATE: I've discovered there's a slightly more advanced version of the ab ripper routine (level 200: 10 exercises, 20 reps.) we do--and it's even viewable on the 'net! Have a look here.
The title pretty much says it all: have I told you everything we do in the way of fitness? No, not everything. I've focused on the major components of our fitness regimen, i.e., the cycling/stationary-bike stuff for aerobic and lower-body strengthening on the one hand, and the strength-training workouts we do for upper body on the other. But there are actually a couple of other fitness routines that we work in, one of which I've not mentioned at all (shame on me).
The one I have mentioned is walking. We do sometimes replace cycling/stationary-bike riding with walking (2 - 8 miles)--as I've pointed out in a previous entry. But what I haven't mentioned is that I additionally try to walk about 1.5 miles on days when we have our strength training (Mon. and Fri.) and also on our rest day (Wed.). It's not much, but with age and being involved in an otherwise sedentary field of work, it's good to get in any extra activity you can. So there's that.
But what I've not mentioned at all is our abdominal workouts. We actually go fairly light on these, spending 5 minutes or so on cycling days performing them. One set of exercises that we do are ones that were given to me by a physical therapist who I was seeing last spring about some back pain. There are some crunches in there, an exercise called "dead bug," another called "mermaid," and another called "bird dog." These are as much core-strengthening exercises as abdominal exercises, though, of course, the two groups of muscles are closely related. Some of the movements remind me somewhat of Pilates exercises.
The other routine we do is one we appropriated from the Power 90 program. It's called "ab ripper 100." And our old friend Tony Horton leads the exercises.
Here's the list of exercises (10 moves, 10 reps each): 1 crunches, 2. left side crunch, 3. right side crunch, 4. elbows to knees, 5. superman crunch, 6. leg lifts, 7. in and outs, 8. hip rock, 9. bicycles, 10. full body crunch.
Using this routine has gone well for us so far--though I do sometimes hurt my back doing ab exercises: both the ab ripper routine and the other set of exercises I got from the physical therapist are liable to cause me lower-back trouble if I don't do them carefully. At the moment, in fact, we're taking a break from all abdominal exercises since I hurt my back about 10 days ago or so. But that hiatus should end soon. As will be evident from the time signature in these still frames, the whole routine only takes about 4.5 minutes
Anyway, I have thought of stepping up the abdominal workouts a bit during part of the year. Currently, I'm considering whether to replace our current abdominal routines with "ab ripper x" (jeez I hate these titles! I think I'll just call it "abdomen firmer" from now on) for part of the year. That's about a 15 minute routine, so it'd be quite a bit more intense than what we do now. But hey, I'm up for doing it for 2 or 3 months out of each year.
That's still in the planning stages, though. Look for further updates on the abdominal exercise front later. And by the way, don't I need to include these abdominal exercises at least somewhere in my overview of our regime? Another note to self: P90X's core synergistics DVD might be a good one to work into the abdominal/core regimen on occasion as well, no?
UPDATE: I've discovered there's a slightly more advanced version of the ab ripper routine (level 200: 10 exercises, 20 reps.) we do--and it's even viewable on the 'net! Have a look here.
Tuesday, January 19, 2010
The reluctant blogger (blood pressure . . . again!)
Ok, I'll admit it. I'm still pretty bummed about my blood pressure results at the doctor's office yesterday. 150/100 was about the best reading I could manage (others were 160+ over 90+). And the readings were pretty much the same in both arms.
This pretty much confirms that the fairly normal reading I got at the doctor's office last Friday was either a mistake, an anomaly, or I misunderstood what the nurse said. Since she only spent about 10 seconds taking my blood pressure, I'm guessing it's the first of those three options. And it does start to look like I can pretty much trust the self-service blood pressure machine at the local pharmacy.
So, what do I do from here? One of the first orders of business is to get back on the hydrochlorothiazide (HZ), which I did yesterday. Looks like there's no other option for now. I've continued with the breathing exercises but I'm reconsidering whether to keep them up: either the medication is going to lower the blood pressure to where it should be or the exercises are. The latter appear thus far to not have been very effective.
There is some anecdotal evidence that can be gleaned from certain web forums that creatine can heighten blood pressure. I'll have to look more carefully into that. But my increased blood pressure does predate my creatine experimentation. By the look of things at present my blood pressure did no change much between the high reading I got some weeks ago (while off HZ) and this week (while also off HZ).
On a somewhat brighter note it seems there might not be such a conflict between creatine and HZ: we uncovered a fairly recent study (2002, if memory serves) that seemed to indicate that creatine is not a diuretic--as has been widely presumed for some time. I will thus see if I can continue the creatine even while taking HZ.
I will also experiment with decreasing the creatine dosage (to something less than 5 grams; maybe 2.5?). I get a kind of buzz from it, oddly enough. Makes me feel a bit jittery--to be expected for a vegetarian I suppose, since I read just today that the most dramatic effects of creatine are to be expected among vegetarians.
I actually have an update to give on creatine. But I'll save it from being overshadowed by the somber tone of this entry and will write about that another day; tomorrow, perhaps?
I've also begun wondering what, if anything, I can do in the way of physical activity in the winter months to bring down my blood pressure. Maybe an hours-long incredibly hard workout once a week--something approximating what I get during the cycling season (though then it's often more than once aweek)--would help? I'll be trying to scheme up a way to do this over the coming days/weeks.
So far I'm not sure how it could be accomplished. I can't see myself putting out that hard on a stationary bike for two or more hours. Anyway, more food for thought.
Until next time . . .
This pretty much confirms that the fairly normal reading I got at the doctor's office last Friday was either a mistake, an anomaly, or I misunderstood what the nurse said. Since she only spent about 10 seconds taking my blood pressure, I'm guessing it's the first of those three options. And it does start to look like I can pretty much trust the self-service blood pressure machine at the local pharmacy.
So, what do I do from here? One of the first orders of business is to get back on the hydrochlorothiazide (HZ), which I did yesterday. Looks like there's no other option for now. I've continued with the breathing exercises but I'm reconsidering whether to keep them up: either the medication is going to lower the blood pressure to where it should be or the exercises are. The latter appear thus far to not have been very effective.
There is some anecdotal evidence that can be gleaned from certain web forums that creatine can heighten blood pressure. I'll have to look more carefully into that. But my increased blood pressure does predate my creatine experimentation. By the look of things at present my blood pressure did no change much between the high reading I got some weeks ago (while off HZ) and this week (while also off HZ).
On a somewhat brighter note it seems there might not be such a conflict between creatine and HZ: we uncovered a fairly recent study (2002, if memory serves) that seemed to indicate that creatine is not a diuretic--as has been widely presumed for some time. I will thus see if I can continue the creatine even while taking HZ.
I will also experiment with decreasing the creatine dosage (to something less than 5 grams; maybe 2.5?). I get a kind of buzz from it, oddly enough. Makes me feel a bit jittery--to be expected for a vegetarian I suppose, since I read just today that the most dramatic effects of creatine are to be expected among vegetarians.
I actually have an update to give on creatine. But I'll save it from being overshadowed by the somber tone of this entry and will write about that another day; tomorrow, perhaps?
I've also begun wondering what, if anything, I can do in the way of physical activity in the winter months to bring down my blood pressure. Maybe an hours-long incredibly hard workout once a week--something approximating what I get during the cycling season (though then it's often more than once aweek)--would help? I'll be trying to scheme up a way to do this over the coming days/weeks.
So far I'm not sure how it could be accomplished. I can't see myself putting out that hard on a stationary bike for two or more hours. Anyway, more food for thought.
Until next time . . .
Sunday, January 17, 2010
The blood pressure problem: a brief history
As you may have noted, I've been writing about blood pressure a lot lately. This is owing, of course, to the fact that high blood pressure was one of the main motivating factors for the fitness regime I've adopted and that I discuss in this blog.
Describing to someone the other day the course of my blood pressure problems, I recalled just how serious things had gotten. I decided after that discussion that I should offer a brief overview of that course of events here in my blog as well so that my readers might better understand some of my motivations for becoming more serious about fitness. Thus, the following.
Throughout my life my blood pressure had been absolutely stable and normal. I can't say that I spent a lot of time in doctors' office prior to the late 1990's or so. In fact, I tried to avoid as much as possible visits to the doctor. And my health was generally good enough that I really didn't seem to require much physician assistance. But I don't recall at any point in my life--prior to just a few years ago--seeing any blood pressure reading above something like 120/75.
I began to make more frequent visits to the doctor's office in the late 90's owing to a health issue that began to plague me then and, consequently, had my blood pressure taken more frequently. And the normal blood pressure readings continued to be the norm until about '05 or so.
I'd say it was about then that I began to notice systolic readings of around 130 or a little higher. Beyond noting that these readings were a bit above what I'd seen throughout my earlier life, I didn't pay much attention to them. And I was not cautioned about it at the time by any medical staff, either.
It was probably one to two years after this that, when on a physician's visit for an unrelated test, I was told that my blood pressure was high and that I should see my doctor about this. Due to the fact that I was then between doctors, I did not manage to make an appointment with a physician in a timely manner.
It was probably at around this same time that I began to occasionally get headaches that seemed to worsen when I was lying down. I had already been experiencing a good deal of insomnia by that point, and the headaches made my insomnia problem even worse: I would simply have to get out of bed after a certain, fairly short period, because my headache was preventing me from sleeping. I didn't initially connect these headches with the blood pressure warning I'd gotten.
Also at around this time another odd health issue developed: I would sometimes get bloody noses for no apparent reason. It would feel as though I had a runny nose, but when I'd wipe my nose, I'd see that the liquid was actually blood. Someone mentioned to me that this might be caused by high blood pressure. But since I hadn't yet selected a new physician, I still did not seek medical attention.
Finally, while out of town on one occasion I was discussing some of my health issues with the wife--who happened also to be a nurse--of a friend of mine. She happened to have blood-pressure-measuring equipment in her home and offered to check my blood pressure, to which I readily agreed. She was shocked at the reading she got--something like 165/110. She essentially demanded that I immediately see a physician.
Trying to determine whether my condition warranted an early return home from that trip, I spoke "off the record" with a doctor who lived in that area. She said tests would be required before any medication could be recommended. But what sticks with me most about that conversation was when she asked "you know what the risk (of going around with high blood pressure) is, right?" When I replied that I did not know the risk, she told me: stroke.
This really drove home the urgency of the matter because I probably simultaneously realized both that I was no longer a young man, and also that I actually know someone who--though seemingly fairly healthy--had a stroke at age 48 (a year younger than my age at the time). I decided to cut my trip short and return home to see the first physician I could get to.
That pretty well summarizes the series of events that proved to be the key motivating factor in getting me on my current fitness regime. I was given tests at that doctor's visit to see what sort of medication I might take to lower the blood pressure and began taking hydrochlorothiazide. And I resolved right away to embark on the fitness regime that I continue to this day.
Summary
A few words, by way of summary, on the effects, to date, of the fitness regime on my blood pressure.
I was uncertain whether adopting this fitness regime would actually "cure" my blood pressure issues. The physician I initially saw about the problem was not encouraging that my issues could be resolved through a more serious fitness regime: instead, he seemed to be urging resignation to the fact that I might well have to take medication for this condition for the remainder of my life.
To be fair, he didn't discourage me from exercising--but he also didn't hold out much hope that my problem could be reversed by this means. It was therefore largely my own initiative to see how I might affect the problem through adopting a more serious exercise regimen. At the least, I was pretty certain it couldn't hurt; at best, I hoped it might bring the problem under control.
And the jury's still out at this point about what the net effect of my 1.75 years of serious fitness endeavors on blood pressure: those who've read my posts about recent blood pressure readings may be aware that I can't say at this point what the net effect has been because I'm now attempting to find out how/when/where I can accurately measure my blood pressure.
I can say with some confidence that, during warm weather when I'm most active, I seem not to need the medicine at all. I'm now trying to determine whether I can remain off the medication for the remainder of this winter.
If so, might I have reversed my condition through exercise? And how might the breathing exercises I've recently adopted--something only tangentially related to my fitness endeavors--have influenced blood pressure readings? I'm still in the process of answering these questions. Please continue reading my blog to find out the answers.
Describing to someone the other day the course of my blood pressure problems, I recalled just how serious things had gotten. I decided after that discussion that I should offer a brief overview of that course of events here in my blog as well so that my readers might better understand some of my motivations for becoming more serious about fitness. Thus, the following.
Throughout my life my blood pressure had been absolutely stable and normal. I can't say that I spent a lot of time in doctors' office prior to the late 1990's or so. In fact, I tried to avoid as much as possible visits to the doctor. And my health was generally good enough that I really didn't seem to require much physician assistance. But I don't recall at any point in my life--prior to just a few years ago--seeing any blood pressure reading above something like 120/75.
I began to make more frequent visits to the doctor's office in the late 90's owing to a health issue that began to plague me then and, consequently, had my blood pressure taken more frequently. And the normal blood pressure readings continued to be the norm until about '05 or so.
I'd say it was about then that I began to notice systolic readings of around 130 or a little higher. Beyond noting that these readings were a bit above what I'd seen throughout my earlier life, I didn't pay much attention to them. And I was not cautioned about it at the time by any medical staff, either.
It was probably one to two years after this that, when on a physician's visit for an unrelated test, I was told that my blood pressure was high and that I should see my doctor about this. Due to the fact that I was then between doctors, I did not manage to make an appointment with a physician in a timely manner.
It was probably at around this same time that I began to occasionally get headaches that seemed to worsen when I was lying down. I had already been experiencing a good deal of insomnia by that point, and the headaches made my insomnia problem even worse: I would simply have to get out of bed after a certain, fairly short period, because my headache was preventing me from sleeping. I didn't initially connect these headches with the blood pressure warning I'd gotten.
Also at around this time another odd health issue developed: I would sometimes get bloody noses for no apparent reason. It would feel as though I had a runny nose, but when I'd wipe my nose, I'd see that the liquid was actually blood. Someone mentioned to me that this might be caused by high blood pressure. But since I hadn't yet selected a new physician, I still did not seek medical attention.
Finally, while out of town on one occasion I was discussing some of my health issues with the wife--who happened also to be a nurse--of a friend of mine. She happened to have blood-pressure-measuring equipment in her home and offered to check my blood pressure, to which I readily agreed. She was shocked at the reading she got--something like 165/110. She essentially demanded that I immediately see a physician.
Trying to determine whether my condition warranted an early return home from that trip, I spoke "off the record" with a doctor who lived in that area. She said tests would be required before any medication could be recommended. But what sticks with me most about that conversation was when she asked "you know what the risk (of going around with high blood pressure) is, right?" When I replied that I did not know the risk, she told me: stroke.
This really drove home the urgency of the matter because I probably simultaneously realized both that I was no longer a young man, and also that I actually know someone who--though seemingly fairly healthy--had a stroke at age 48 (a year younger than my age at the time). I decided to cut my trip short and return home to see the first physician I could get to.
That pretty well summarizes the series of events that proved to be the key motivating factor in getting me on my current fitness regime. I was given tests at that doctor's visit to see what sort of medication I might take to lower the blood pressure and began taking hydrochlorothiazide. And I resolved right away to embark on the fitness regime that I continue to this day.
Summary
A few words, by way of summary, on the effects, to date, of the fitness regime on my blood pressure.
I was uncertain whether adopting this fitness regime would actually "cure" my blood pressure issues. The physician I initially saw about the problem was not encouraging that my issues could be resolved through a more serious fitness regime: instead, he seemed to be urging resignation to the fact that I might well have to take medication for this condition for the remainder of my life.
To be fair, he didn't discourage me from exercising--but he also didn't hold out much hope that my problem could be reversed by this means. It was therefore largely my own initiative to see how I might affect the problem through adopting a more serious exercise regimen. At the least, I was pretty certain it couldn't hurt; at best, I hoped it might bring the problem under control.
And the jury's still out at this point about what the net effect of my 1.75 years of serious fitness endeavors on blood pressure: those who've read my posts about recent blood pressure readings may be aware that I can't say at this point what the net effect has been because I'm now attempting to find out how/when/where I can accurately measure my blood pressure.
I can say with some confidence that, during warm weather when I'm most active, I seem not to need the medicine at all. I'm now trying to determine whether I can remain off the medication for the remainder of this winter.
If so, might I have reversed my condition through exercise? And how might the breathing exercises I've recently adopted--something only tangentially related to my fitness endeavors--have influenced blood pressure readings? I'm still in the process of answering these questions. Please continue reading my blog to find out the answers.
Saturday, January 16, 2010
Intervals continued
Just a short entry today to comment on how I continue to be pleased with the interval training we're doing on the stationary bikes. I really like it--more interesting than simply riding at a steady pace for the same amount of time.
Tonight we managed to get in only about 5 intervals due to interruptions. So probably total time on the bikes was 15 to 20 minutes. It's going to be hard to go back to just spinning for a half hour. But who knows, maybe I'll get sick of intervals at some point?
(This setup is something like what I'm riding except I've replaced my front wheel with an upright 2x4)
Friday, January 15, 2010
Blood pressure saga continued: part 1 of ?
Well, well. I don't know whether to be pleased or disappointed this morning. I've been off the blood pressure meds for a little over a week now so that I could complete the "loading phase" of creatine supplementation (read more about that here). A blood pressure reading gotten from a self-service blood pressure reading machine earlier this week--152/94 (left arm)--had me a little concerned. Today, however--only 2 days later--I get quite a different, greatly improved reading, at my doctor's office: 122/84 (right arm).
WTF? (excuse my French). Let the trouble-shooting begin.
I actually began trouble-shooting immediately by heading straight from the doctor's office to the self-service machine at the pharmacy. By the time I had walked there (about 1 mile) and taken my blood pressure again (left arm), am I to believe that my systolic pressure had gone up by something like 34 points, and my diastolic by 10 (the two readings I got at the pharmacy's machine were 159/94 and 140/90)? Something began to smell a little fishy . . .
Though my immediate inclination is to trust the doctor's office reading over the self-service machine's readings, here are some things I'm taking into consideration as I attempt to figure out what's going on and which is right. 1) it is possible to get different readings from each arm: how much variation should be expected is something I have yet to determine. But I have to say I'm highly skeptical from the outset that such wildly differing readings could be gotten from the arms of any reasonably healthy individual--aka me. 2) self-service blood pressure machines are not to be implicitly trusted. As we read on the Mayo clinic web site, these machines are "Not accurate enough to make health decisions regarding your blood pressure." 3) I've adjusted my breathing exercises since the 152/94 reading and am now doing them in closer conformity to the recommendations I've read. I do feel a better effect from these exercises when using the recommended method (twice as long to exhale as to inhale) than I felt using the less precise method I had followed previously.
Regarding 1): the self-service machine offers no possibility for measuring blood pressure in the right arm, so I have no way of testing whether I might get, using it, widely disparate readings from the two arms. I intend to address the matter by asking, next time I have my blood pressure measured at the doctor's office, that they measure it twice--once on each arm. That will give me a better idea whether there is a wide disparity in pressure between the two arms.
Finding out about that will help me to determine something about issue 2): if blood pressure readings from both arms are about the same, that will be one probable indicator that the self-service machine is poorly calibrated. Furthermore, if the blood pressure taken at the doctor's office from both arms is as close to the normal range as the reading I got at the doctor's office today using my right arm, there will be yet more reason to suspect the self-service machine is not to be trusted. To make an even more definitive judgment on this, I should run by the drugstore on my way home from the doctor's office and check and compare the blood pressure reading I get there with the readings I got from the doctor. If the pressure taken in both arms at the doctor's office is almost the same, and if it is substantially lower than the reading gotten from the self-service machine, it would be reasonable to conclude that this machine is simply untrustworthy and should be avoided.
Results from 1) and 2) above will not, unfortunately, help me to determine anything definite about issue 3). I might be able to guess after conducting the tests outlined above that the 152/92 reading I got from the self-service machine a couple of days ago was erroneous and, furthermore, that it was perhaps significantly higher than my actual blood pressure at the time. But that will remain speculation and will not provide me with evidence that the new breathing technique has helped to lower my blood pressure. In that case, I would simply have to rely on subjective impressions and say, since I've noted a greater feeling of relief and calmness in connection with the new breathing exercise pattern, that it is likely helping to lower my blood pressure.
Part 2 of this series on the blood pressure saga will, I hope, resolve some of these monumental dilemmas. Stay tuned for the next episode of . . . what's my real blood pressure!
WTF? (excuse my French). Let the trouble-shooting begin.
I actually began trouble-shooting immediately by heading straight from the doctor's office to the self-service machine at the pharmacy. By the time I had walked there (about 1 mile) and taken my blood pressure again (left arm), am I to believe that my systolic pressure had gone up by something like 34 points, and my diastolic by 10 (the two readings I got at the pharmacy's machine were 159/94 and 140/90)? Something began to smell a little fishy . . .
Though my immediate inclination is to trust the doctor's office reading over the self-service machine's readings, here are some things I'm taking into consideration as I attempt to figure out what's going on and which is right. 1) it is possible to get different readings from each arm: how much variation should be expected is something I have yet to determine. But I have to say I'm highly skeptical from the outset that such wildly differing readings could be gotten from the arms of any reasonably healthy individual--aka me. 2) self-service blood pressure machines are not to be implicitly trusted. As we read on the Mayo clinic web site, these machines are "Not accurate enough to make health decisions regarding your blood pressure." 3) I've adjusted my breathing exercises since the 152/94 reading and am now doing them in closer conformity to the recommendations I've read. I do feel a better effect from these exercises when using the recommended method (twice as long to exhale as to inhale) than I felt using the less precise method I had followed previously.
Regarding 1): the self-service machine offers no possibility for measuring blood pressure in the right arm, so I have no way of testing whether I might get, using it, widely disparate readings from the two arms. I intend to address the matter by asking, next time I have my blood pressure measured at the doctor's office, that they measure it twice--once on each arm. That will give me a better idea whether there is a wide disparity in pressure between the two arms.
Finding out about that will help me to determine something about issue 2): if blood pressure readings from both arms are about the same, that will be one probable indicator that the self-service machine is poorly calibrated. Furthermore, if the blood pressure taken at the doctor's office from both arms is as close to the normal range as the reading I got at the doctor's office today using my right arm, there will be yet more reason to suspect the self-service machine is not to be trusted. To make an even more definitive judgment on this, I should run by the drugstore on my way home from the doctor's office and check and compare the blood pressure reading I get there with the readings I got from the doctor. If the pressure taken in both arms at the doctor's office is almost the same, and if it is substantially lower than the reading gotten from the self-service machine, it would be reasonable to conclude that this machine is simply untrustworthy and should be avoided.
Results from 1) and 2) above will not, unfortunately, help me to determine anything definite about issue 3). I might be able to guess after conducting the tests outlined above that the 152/92 reading I got from the self-service machine a couple of days ago was erroneous and, furthermore, that it was perhaps significantly higher than my actual blood pressure at the time. But that will remain speculation and will not provide me with evidence that the new breathing technique has helped to lower my blood pressure. In that case, I would simply have to rely on subjective impressions and say, since I've noted a greater feeling of relief and calmness in connection with the new breathing exercise pattern, that it is likely helping to lower my blood pressure.
Part 2 of this series on the blood pressure saga will, I hope, resolve some of these monumental dilemmas. Stay tuned for the next episode of . . . what's my real blood pressure!
Thursday, January 14, 2010
Gross-out warning: intense exercise and the retch factor
Here's an entry about a long-standing problem I've had in my athletic pursuits. It relates to my current exercise endeavors in that, for me, exercise means, by definition, strain and heightened effort.
Did you ever get the feeling during your workout that you were on the verge of vomiting? I sure have. It happens to me all the time and my efforts at preventing myself from dumping lunch regularly cause me to curtail my output.
Back in my bicycle racing days one of the things--apart from the rather lackadaisical approach I took to training--that kept me from doing better was, I think, the way my digestive system was malfunctioning. To be more particular, I often found that when I would try to explode my effort, as is often required in a race if you don't want to get dropped, my stomach would go into rebellion.
 What would happen very regularly shortly after I'd begin to put out maximum effort is that my esophagus would begin to burn intensely: it was as if hot coals were trying to force their way out of my stomach and out through my esophagus to issue in a fiery stream of vomit (yeah, that's a picture of me on the right, finally relieving the pent up pressure as I cross the finish line of a race that took me about 6 hours longer than everyone else to finish . . . just kidding!). It's a sick image, I know. But I had that sensation on many, many occasions when racing or on hard training rides.
What would happen very regularly shortly after I'd begin to put out maximum effort is that my esophagus would begin to burn intensely: it was as if hot coals were trying to force their way out of my stomach and out through my esophagus to issue in a fiery stream of vomit (yeah, that's a picture of me on the right, finally relieving the pent up pressure as I cross the finish line of a race that took me about 6 hours longer than everyone else to finish . . . just kidding!). It's a sick image, I know. But I had that sensation on many, many occasions when racing or on hard training rides.
The accompanying sensation of feeling as though stomach contents are about to eject and the corollary reaction of trying to keep that from happening has, let's say, a negative effect on effort. With respect to a highly aerobic sport like cycling its impact is very signficant: the attempt to suppress regurgitation disrupts breathing patterns in a major way--and just at a time when your leg muscles are crying out for maximal amounts of oxygen. It's hard to compete seriously in that state.
I never asked my fellow racers whether they'd ever experienced such a thing but I wish I had. My guess is that, while every serious athlete will regurgitate from exertion at some point--usually in conjunction with having eaten too close to the start of an event or a difficult workout--they probably did not have either the burning sensation or experience the regurgitative impulse as frequently as I have.
These bouts, along with some other stomach issues I experience, led me later to theorize that I probably have a hiatal hernia. It remains a theory, though. I did have an endoscopy some years ago and, when I mentioned my theory about the hiatal hernia to the doctor that performed the procedure, he said he hadn't seen signs of one. But I am unconvinced.
Be that as it may I bring up this longstanding issue now because, with my renewed fitness efforts, I'm once again confronting this old problem. It comes up when we cycle in the summer and I'm riding hardest. I'd say the burning sensation I get is proportional to the effort I'm expending, but even when I don't have that intense burning sensation, I do nonetheless feel as though I'm on the verge of barfing.
And I'm getting this feeling during our strength-training workouts as well. In fact, it's begun to plague me to the extent that I have to eat a very light lunch on strength-training days so as to be able to not feel nauseous during the latter part of the workout. It's especially bothersome with moves like incline push-ups but any exercise that involves being prone or bent over can exacerbate it. I've begun to realize just how much the attempt to suppress regurgitation takes out of my overall effort: it's kind of hard to give it your all when part of you is struggling to keep stomach contents down.
It's kind of a gross subject but something I need to address and figure out how to deal with. The simple solution is to be very careful about how and when I eat in relation to the workout. That's easy enough to do with strength-training workouts which are relatively short. With cycling it's harder since we're often out for several hours: you need to have some decent calories in your system before departing.
The odd thing in my experience is that, even 5 or 6 hours after I've eaten I can still get this sensation of stomach contents trying to breach their gastric confines. In the case of our strength training, for example, I'm trying to eat no closer than 6 hours before the workout. I feel and do so much better when I don't have to suppress the urge to toss my cookies. But it does take some will power to keep from snacking closer to the workout.
My latest idea is to try having a "super shake" for lunch on strength-training days, perhaps even an extra large one, a portion of which I'll save for a small snack a little later in the afternoon. I'll try that in the coming days to see what are the results. But when it comes to cycling season and those long rides, the problem will become harder to address.
Anyone care to share their gross-out experiences with working out or athletics and the retch factor?
Did you ever get the feeling during your workout that you were on the verge of vomiting? I sure have. It happens to me all the time and my efforts at preventing myself from dumping lunch regularly cause me to curtail my output.
Back in my bicycle racing days one of the things--apart from the rather lackadaisical approach I took to training--that kept me from doing better was, I think, the way my digestive system was malfunctioning. To be more particular, I often found that when I would try to explode my effort, as is often required in a race if you don't want to get dropped, my stomach would go into rebellion.
 What would happen very regularly shortly after I'd begin to put out maximum effort is that my esophagus would begin to burn intensely: it was as if hot coals were trying to force their way out of my stomach and out through my esophagus to issue in a fiery stream of vomit (yeah, that's a picture of me on the right, finally relieving the pent up pressure as I cross the finish line of a race that took me about 6 hours longer than everyone else to finish . . . just kidding!). It's a sick image, I know. But I had that sensation on many, many occasions when racing or on hard training rides.
What would happen very regularly shortly after I'd begin to put out maximum effort is that my esophagus would begin to burn intensely: it was as if hot coals were trying to force their way out of my stomach and out through my esophagus to issue in a fiery stream of vomit (yeah, that's a picture of me on the right, finally relieving the pent up pressure as I cross the finish line of a race that took me about 6 hours longer than everyone else to finish . . . just kidding!). It's a sick image, I know. But I had that sensation on many, many occasions when racing or on hard training rides.The accompanying sensation of feeling as though stomach contents are about to eject and the corollary reaction of trying to keep that from happening has, let's say, a negative effect on effort. With respect to a highly aerobic sport like cycling its impact is very signficant: the attempt to suppress regurgitation disrupts breathing patterns in a major way--and just at a time when your leg muscles are crying out for maximal amounts of oxygen. It's hard to compete seriously in that state.
I never asked my fellow racers whether they'd ever experienced such a thing but I wish I had. My guess is that, while every serious athlete will regurgitate from exertion at some point--usually in conjunction with having eaten too close to the start of an event or a difficult workout--they probably did not have either the burning sensation or experience the regurgitative impulse as frequently as I have.
These bouts, along with some other stomach issues I experience, led me later to theorize that I probably have a hiatal hernia. It remains a theory, though. I did have an endoscopy some years ago and, when I mentioned my theory about the hiatal hernia to the doctor that performed the procedure, he said he hadn't seen signs of one. But I am unconvinced.
Be that as it may I bring up this longstanding issue now because, with my renewed fitness efforts, I'm once again confronting this old problem. It comes up when we cycle in the summer and I'm riding hardest. I'd say the burning sensation I get is proportional to the effort I'm expending, but even when I don't have that intense burning sensation, I do nonetheless feel as though I'm on the verge of barfing.
And I'm getting this feeling during our strength-training workouts as well. In fact, it's begun to plague me to the extent that I have to eat a very light lunch on strength-training days so as to be able to not feel nauseous during the latter part of the workout. It's especially bothersome with moves like incline push-ups but any exercise that involves being prone or bent over can exacerbate it. I've begun to realize just how much the attempt to suppress regurgitation takes out of my overall effort: it's kind of hard to give it your all when part of you is struggling to keep stomach contents down.
It's kind of a gross subject but something I need to address and figure out how to deal with. The simple solution is to be very careful about how and when I eat in relation to the workout. That's easy enough to do with strength-training workouts which are relatively short. With cycling it's harder since we're often out for several hours: you need to have some decent calories in your system before departing.
The odd thing in my experience is that, even 5 or 6 hours after I've eaten I can still get this sensation of stomach contents trying to breach their gastric confines. In the case of our strength training, for example, I'm trying to eat no closer than 6 hours before the workout. I feel and do so much better when I don't have to suppress the urge to toss my cookies. But it does take some will power to keep from snacking closer to the workout.
My latest idea is to try having a "super shake" for lunch on strength-training days, perhaps even an extra large one, a portion of which I'll save for a small snack a little later in the afternoon. I'll try that in the coming days to see what are the results. But when it comes to cycling season and those long rides, the problem will become harder to address.
Anyone care to share their gross-out experiences with working out or athletics and the retch factor?
Wednesday, January 13, 2010
Important flash: cold weather and increased blood pressure!
I'm not very happy with my blood pressure reading today--152/94 is pretty high. I think if I were to go back on hydrochlorothiazide (HZ hereafter) it would decrease to something closer to the normal range. But I want to try and stick it out without the meds at least until my "loading phase" with creatine is finished (in two days).
As far as my blood pressure going up in the cycling off-season, I stumbled across some relevant information yesterday. While researching high blood pressure I found this tidbit:
You'd probably have to see me on the bike to appreciate what I'm saying, but I'm telling you I put out major energy--and I'm not talking about over a mere 40 minute span; no, 40 minutes is the minimum. I can go like that for 1, 2, 3--maybe even as long as 5 hours of really intense output.
To make numerical a comparison, I work pretty hard during our strength-training sessions and always have worked up a good sweat by the end--despite having the fan blowing on me. But I've worn my heart rate monitor while doing strength training and my heart rate rarely goes over 140 BPM. By contrast, on the bike it's routine for me to sustain a heart rate in the 150's BPM for a half hour or more, and I'm often taking that up further yet to 160-170 BPM on hills. I'm certain this type of intense and extended aerobic activity has an effect on blood pressure, though I'm willing to concede that temperature could have its effect in addition.
As far as my blood pressure going up in the cycling off-season, I stumbled across some relevant information yesterday. While researching high blood pressure I found this tidbit:
QuestionHave I discovered the reason why I am able to pretty much cease taking HZ when the weather's warm? I can't believe warm temperature is solely responsible for the lower blood pressures I see in the summer.
Blood pressure: Is it affected by cold weather?
Can weather affect blood pressure? I've noticed that my blood pressure is harder to control in the winter.
Answer
from Sheldon G. Sheps, M.D.
Yes, weather can affect blood pressure. Blood pressure generally is higher in the winter and lower in the summer. Why? Cold temperatures cause your blood vessels to narrow (constrict) — which increases blood pressure because more pressure is needed to force blood through a narrower space. Other possible causes of higher blood pressure are weight gain and decreased physical activity in winter.
However, it doesn't take a big cold snap to raise blood pressure. Seasonal blood pressure changes also are found in climates where temperatures may change only a few degrees from summer to winter. In fact, a five-year analysis of the electronic health records of 444,000 adults with high blood pressure in the United States and its territories found that high blood pressure was less controlled in winter than in summer in all cities, from Anchorage, Alaska, to San Juan, Puerto Rico. The implication from such studies is that it may be necessary to adjust high blood pressure medications in some people to continue to control blood pressure in different seasons.
If you have questions about how weather may affect your blood pressure, consult your doctor.
You'd probably have to see me on the bike to appreciate what I'm saying, but I'm telling you I put out major energy--and I'm not talking about over a mere 40 minute span; no, 40 minutes is the minimum. I can go like that for 1, 2, 3--maybe even as long as 5 hours of really intense output.
To make numerical a comparison, I work pretty hard during our strength-training sessions and always have worked up a good sweat by the end--despite having the fan blowing on me. But I've worn my heart rate monitor while doing strength training and my heart rate rarely goes over 140 BPM. By contrast, on the bike it's routine for me to sustain a heart rate in the 150's BPM for a half hour or more, and I'm often taking that up further yet to 160-170 BPM on hills. I'm certain this type of intense and extended aerobic activity has an effect on blood pressure, though I'm willing to concede that temperature could have its effect in addition.
Labels:
blood pressure,
bpm,
cycling,
heart rate,
hydrochlorothiazide
Tuesday, January 12, 2010
Current and past weekly routines
I'm on kind of a table craze lately. My latest idea is to post a table that will offer a concise overview of our past and current fitness endeavors by weekday. As you can see, cycling/stationary bike riding is the mainstay of our fitness program.1
Thus, the following table that lists our fitness pursuits by typical week2 since April of 2008:
To be updated as our routine changes.
ADDENDUM: Thinking today about our regime I realized that, at certain parts of the year, we might be doing as little as about 2 hours per week of exercise. Of course we do try to be active during those periods in other ways, such as by sometimes walking instead of driving and taking the stairs instead of the elevator--so it's not as if we're totally sedentary the other 166 hours of the week. Then again, during a different part of the year (height of the cycling season) we might get in 14 hours or more of fitness activities during a given week. And we also do some walking and stair-climbing during this portion of the year as well.
-----------------------
1 As mentioned in this entry, on-street cycling sessions (done when weather permits) range from .5 hours to 7 hours. Stationary bike sessions run 20-30 minutes--the 30-minute sessions usually being cardio workouts aiming to raise and sustain the cardio-vascular rate for the designated period, while the 20-minute sessions typically involve a recurring pattern of 30-second intense riding intervals followed by 3-minutes of liesurely spinning recovery (as described in this entry).
2 We do occassionally miss a day. In addition we've so far taken periods of anywhere from one week to one month off at certain points in the year due to religious or other obligations or vacations. This sort of intentional break might occur 3 to 4 times in total in a given year.
3 We also try to work in several minutes of abdominal/core exercises on these days.
4 It might be a bit confusing that I call this the "arm toner phase" while listing the Monday and Friday exercise routine as "modified Power 1/2 hr." in the table. To provide a simple explanation, we excerpt from the Power Half Hour program a routine called "Arm Toner," which we do on Mondays and Fridays during this phase.
Thus, the following table that lists our fitness pursuits by typical week2 since April of 2008:
| Sunday3 | Monday | Tuesday3 | Wednesday | Thursday | Friday | Saturday |
|---|---|---|---|---|---|---|
| cycling/stat. bike | cycling/stat. bike | rest day | cycling/stat. bike | cycling/stat. bike | ||
| cycling/stat. bike | modified Power 1/2 hr. | cycling/stat. bike | rest day | cycling/stat. bike | modified Power 1/2 hr. | cycling/stat. bike |
| cycling/stat. bike | modified Power90 | cycling/stat. bike | rest day | cycling/stat. bike | modified Power90 | cycling/stat. bike |
| cycling/stat. bike | rest day | cycling/stat. bike | alternate modified P90X | cycling/stat. bike | rest day | cycling/stat. bike |
| cycling/stat. bike | modified Power 1/2 hr. | cycling/stat. bike | rest day | cycling/stat. bike | modified Power 1/2 hr. | cycling/stat. bike |
| cycling/stat. bike | modified Power90 | cycling/stat. bike | rest day | cycling/stat. bike | modified Power90 | cycling/stat. bike |
| cycling/stat. bike | modified P90X | cycling/stat. bike | rest day | cycling/stat. bike | modified P90X | cycling/stat. bike |
| cycling/stat. bike | Soloflex/calisth. | cycling/stat. bike | rest day | cycling/stat. bike | Soloflex/calisth. | cycling/stat. bike |
To be updated as our routine changes.
ADDENDUM: Thinking today about our regime I realized that, at certain parts of the year, we might be doing as little as about 2 hours per week of exercise. Of course we do try to be active during those periods in other ways, such as by sometimes walking instead of driving and taking the stairs instead of the elevator--so it's not as if we're totally sedentary the other 166 hours of the week. Then again, during a different part of the year (height of the cycling season) we might get in 14 hours or more of fitness activities during a given week. And we also do some walking and stair-climbing during this portion of the year as well.
-----------------------
1 As mentioned in this entry, on-street cycling sessions (done when weather permits) range from .5 hours to 7 hours. Stationary bike sessions run 20-30 minutes--the 30-minute sessions usually being cardio workouts aiming to raise and sustain the cardio-vascular rate for the designated period, while the 20-minute sessions typically involve a recurring pattern of 30-second intense riding intervals followed by 3-minutes of liesurely spinning recovery (as described in this entry).
2 We do occassionally miss a day. In addition we've so far taken periods of anywhere from one week to one month off at certain points in the year due to religious or other obligations or vacations. This sort of intentional break might occur 3 to 4 times in total in a given year.
3 We also try to work in several minutes of abdominal/core exercises on these days.
4 It might be a bit confusing that I call this the "arm toner phase" while listing the Monday and Friday exercise routine as "modified Power 1/2 hr." in the table. To provide a simple explanation, we excerpt from the Power Half Hour program a routine called "Arm Toner," which we do on Mondays and Fridays during this phase.
Labels:
cycling,
intervals,
modified P90X,
modified Power 90,
stationary bike
Monday, January 11, 2010
Breathing exercise table
I've decided to keep track of my breathing exercises in this blog, at least for a time--thus the table below. This table will provide me (and perhaps you) with some important data about whether/how well these breathing exercises can help to lower or control blood pressure.
The table should be pretty self-explanatory. I'll be maintaining this table for as long as I'm off the blood pressure meds (hydrochlorothiazide). In the far right column I will write "n/a" on those days (probably most days) when I was unable to measure my blood pressure. I will provide a link directly to this post among those along the right side of my blog's main page.
------------------------------
UPDATES
1 I decided to start using a stop watch as opposed to a wristwatch for timing these exercises and noted that, contrary to the advice commonly given for executing these breathing exercises--the recommendation being that exhalation should take about twice as long as inhalation--my exhalations were actually taking about 5 times longer than inhalations. So partway through today's exercise I made some adjustments, inhaling more slowly and exhaling a little more quickly. I found a 5 second inhalation followed by a 10 second exhalation to be a pretty comfortable rate. That's what I'll be trying to train myself to do from henceforward, so expect the sub-4 BrPM figures to give way to a steady 4-plus-a-little BrPM rate. Subsequent to today (1/14/10), unless otherwise noted, expect all future entries to follow this new breathing pattern.
2 !!! This reading, as you may guess, warrants comment. The reading was taken at my Dr.'s office, using my right arm. The much higher reading listed above in this table I got from a self-service machine at the local pharmacy using my left arm. The disparity between these readings calls for enough further discussion that I'll limit what I say about it in this note. Look for a subsequent blog entry that will address the details. I'll just mention in parting that, right after getting the 122/84 blood pressure reading, I walked over to the local pharmacy to see what reading I'd get there. So about 1/2 hour later I got readings of 159/90 and 140/90--again using my left arm--from the self-service machine at the pharmacy. UPDATE (1/18/10) I now believe the 122/84 reading was in error and that the actual reading was significantly higher.
3 Taken at the doctor's office. Both arms. Went back on HZ today as a result breathing exercises, at leats in the short term, do not seem to be having much effect. Not sure whether I'll continue with them, and thus this chart.
4 Right arm, taken at doctor's office. After leaving the doctor's office I took readings at the self-service machine in the local pharamacy (left arm) and got similar readings (143/80, 129/84).
5 Pulse 60. Rough night last night. Consequently I got up at the last moment and didn't do breathing exercises which, I'm fairly certain, would have lowered the diastolic reading. The designation "in-house" in this chart will mean the reading was taken here in the building by a nurse who visits about once a month.
6 Was out of town for a few days and did not do breathing exercises with regularity. Finally got back to it today.
The table should be pretty self-explanatory. I'll be maintaining this table for as long as I'm off the blood pressure meds (hydrochlorothiazide). In the far right column I will write "n/a" on those days (probably most days) when I was unable to measure my blood pressure. I will provide a link directly to this post among those along the right side of my blog's main page.
| Date, time | No. of breaths, total time | BrPM average | BP reading, time, where, etc |
|---|---|---|---|
| 1/11/10, 11 AM | 50, 12.5 minutes | 4 | n/a |
| 1/11/10, 11 PM | 50, 14 minutes | ca. 3.6 | n/a |
| 1/12/10, 9 AM | 40, 11 minutes | ca. 3.6 | n/a |
| 1/12/10, 11 PM | 50, 13 minutes | ca. 3.9 | 152/94 (6 PM) |
| 1/13/10, 10 AM | 50, 13 minutes | ca. 3.9 | n/a |
| 1/13/10 11 PM | 37, 10 minutes | 3.7 | n/a |
| 1/14/10 11 AM | 47, 12 minutes | ca. 3.91 | n/a |
| 1/14/10 11:30 PM | 48, 12 minutes | 4 | n/a |
| 1/15/10 8 AM | 40, 10 minutes | 4 | 122/842 |
| 1/15/10 12:30 AM | 44, 11 minutes | 4 | n/a |
| 1/16/10 12:30 PM | 40, 10 minutes | 4 | n/a |
| 1/16/10 12:30 AM | 40, 10 minutes | 4 | n/a |
| 1/17/10 11 PM | 40, 10 minutes | 4 | n/a |
| 1/18/10 8 AM | 40, 10 minutes | 4 | 150/100 (2:30 PM)3 |
| 1/18/10 11 PM | 48, 12 minutes | 4 | n/a |
| 1/19/10 11AM | 40, 10 minutes | 4 | n/a |
| 1/19/10 12 AM | 40, 10 minutes | 4 | n/a |
| 1/20/10 11 AM | 40, 10 minutes | 4 | n/a |
| 1/20/10 12 AM | 40, 10 minutes | 4 | n/a |
| 1/21/10 10:50 AM | 40, 10 minutes | 4 | n/a |
| 1/21/10 10:15 PM | 40, 10 minutes | 4 | n/a |
| 1/22/10 9 AM | 40, 10 minutes | 4 | 130/84 (10 AM)4 |
| 1/23/10 11:30 PM | 40, 10minutes | 4 | n/a |
| 1/24/10 11 PM | 40, 10 minutes | 4 | n/a |
| 1/25/10, 9 AM | 48, 12 minutes | 4 | 131/84, (8:30 AM, pharm., r. arm) |
| 1/25/10 11 PM | 40, 10 minutes | 4 | n/a |
| 1/26/10 4 PM | 40, 10 minutes | 4 | n/a |
| 1/27/10 10:30 PM | 40, 10 minutes | 4 | 132/100 (8 AM, in-house, l. arm)5 |
| 1/28/10 10 AM | 40, 10 minutes | 4 | n/a |
| 1/28/10 11 PM | 40, 10 minutes | 4 | n/a |
| 1/29/10, 11 PM | 40, 10 minutes | 4 | n/a |
| 1/30/10 11 PM | 40, 10 minutes | 4 | n/a |
| 1/31/10, 11 PM | 40, 10 minutes | 4 | n/a |
| 2/1/10, 9 AM | 40, 10 minutes | 4 | n/a |
| 2/2/10 9 AM | 40, 10 minutes | 4 | n/a |
| 2/4/10 11 PM | 40, 10 minutes | 4 | n/a |
| 2/5/10 8:45 AM | 48, 12 minutes | 4 | 128/82 (9 AM, Dr.'s office, r. arm) |
| 2/6/10 11 PM | 40, 10 minutes | 4 | n/a |
| 2/7/10 11 PM | 40, 10 minutes | 4 | n/a |
| 2/8/10 10 PM | 40, 10 minutes | 4 | n/a |
| 2/9/10 10 AM | 40, 10 minutes | 4 | n/a |
| 2/10/10 10:30 AM | 40, 10 minutes | 4 | n/a |
| 2/10/10 11 PM | 40, 10 minutes | 4 | n/a |
| 2/11/10 10 PM | 40, 10 mintes | 4 | n/a |
| 2/12/10 11 AM | 40, 10 minutes | 4 | n/a |
| 2/12/11 PM | 40, 10 minutes | 4 | 134/87 (5 PM, pharm., l. arm) |
| 2/13/10 11 PM | 40, 10 minutes | 4 | n/a |
| 2/14/10 9 AM | 40, 10 minutes | 4 | n/a |
| 2/14/10 11 PM | 40, 10 minutes | 4 | n/a |
| 2/19/10 9 AM | 40, 10 minutes | 4 | 136/86 (9 AM, r. arm, Dr.'s office) |
| 2/20/10, 11 PM | 40, 10 minutes | 4 | n/a |
| 2/21/10 11 PM | 40, 10 minutes | 4 | n/a |
| 2/22/10 10:30 PM | 40, 10 minutes | 4 | n/a |
| 2/23/10 7 AM | 40, 10 minutes | 4 | n/a |
| 3/1/10 11 PM | 40, 10 minutes | 4 | n/a6 |
| 3/5/10 11 AM | 48, 12 minutes | 4 | 150/87 (11 AM, r. arm, Dr.'s office) |
| 3/6/10 11 PM | 40, 10 minutes | 4 | n/a |
| 3/7/10, 11 PM | 40, 10 minutes | 4 | n/a |
| 3/8/10, 11 PM | 40, 10 minutes | 4 | n/a |
| 3/10/10 11 PM | 40, 10 minutes | 4 | n/a |
| 3/11/10 9 AM | 40, 10 minutes | 4 | n/a |
| 3/11/10 11 PM | 40, 10 minutes | 4 | n/a |
| 3/12/10 11 PM | 40, 10 minutes | 4 | n/a |
| 3/13/10 11 PM | 40, 10 minutes | 4 | n/a |
| 3/14/10 11 PM | 40, 10 minutes | 4 | n/a |
| 3/15/10 10 PM | 40, 10 minutes | 4 | n/a |
| 3/22/10 11 AM | 40, 10 minutes | 4 | n/a |
| 3/22/10 10 PM | 40, 10 minutes | 4 | n/a |
| 3/23/10, 10 PM | 40, 10 minutes | 4 | n/a |
| 3/24/10 10 AM | 40, 10 minutes | 4 | 138/98 (11 AM, in-house, r. arm) |
| 3/28/10 | n/a | n/a | 143/84 (6 PM, pharm., l. arm) |
Below are just some empty cells/rows I can copy and paste into the above table, just in case I need them.
------------------------------
UPDATES
1 I decided to start using a stop watch as opposed to a wristwatch for timing these exercises and noted that, contrary to the advice commonly given for executing these breathing exercises--the recommendation being that exhalation should take about twice as long as inhalation--my exhalations were actually taking about 5 times longer than inhalations. So partway through today's exercise I made some adjustments, inhaling more slowly and exhaling a little more quickly. I found a 5 second inhalation followed by a 10 second exhalation to be a pretty comfortable rate. That's what I'll be trying to train myself to do from henceforward, so expect the sub-4 BrPM figures to give way to a steady 4-plus-a-little BrPM rate. Subsequent to today (1/14/10), unless otherwise noted, expect all future entries to follow this new breathing pattern.
2 !!! This reading, as you may guess, warrants comment. The reading was taken at my Dr.'s office, using my right arm. The much higher reading listed above in this table I got from a self-service machine at the local pharmacy using my left arm. The disparity between these readings calls for enough further discussion that I'll limit what I say about it in this note. Look for a subsequent blog entry that will address the details. I'll just mention in parting that, right after getting the 122/84 blood pressure reading, I walked over to the local pharmacy to see what reading I'd get there. So about 1/2 hour later I got readings of 159/90 and 140/90--again using my left arm--from the self-service machine at the pharmacy. UPDATE (1/18/10) I now believe the 122/84 reading was in error and that the actual reading was significantly higher.
3 Taken at the doctor's office. Both arms. Went back on HZ today as a result breathing exercises, at leats in the short term, do not seem to be having much effect. Not sure whether I'll continue with them, and thus this chart.
4 Right arm, taken at doctor's office. After leaving the doctor's office I took readings at the self-service machine in the local pharamacy (left arm) and got similar readings (143/80, 129/84).
5 Pulse 60. Rough night last night. Consequently I got up at the last moment and didn't do breathing exercises which, I'm fairly certain, would have lowered the diastolic reading. The designation "in-house" in this chart will mean the reading was taken here in the building by a nurse who visits about once a month.
6 Was out of town for a few days and did not do breathing exercises with regularity. Finally got back to it today.
Sunday, January 10, 2010
Creatine, intervals, breathing exercises
Here's a fitness update so I can keep up the posting momentum on this blog. I decided I really had nothing to lose by trying out creatine, so I started on that this past week--fuller report below on the effects so far. As a result of trying out creatine, I've gotten more serious and regular about my breathing exercises and once again stopped taking the blood pressure meds: more on that below as well. And finally, we've now started working interval training into our stationary bike sessions--see below for some greater detail on that also.
First thing to report on is creatine. I decided to just buy a small quantity and try it out for awhile. As you will be aware if you read my previous post, I'm hoping as much for a mental benefit from this as I for physical benefits.
Here's how it's going so far. I decided after doing some reading on the topic that, initially, I should take a larger dose of the creatine. So, for the first week--which will end this coming Thursday--I'm taking ca. 15 grams a day.* After that I'll cut down to the more normal daily dosage of about 5 grams daily.
We've only done one strength-training workout since I started this and I would say that so far I've noticed zero effect from the creatine so far as endurance or recovery are concerned. It's too early to say definitively whether it will have much effect in those areas but I can at least say that the initial impression I have is that it's unlikely to have any dramatic effect. That said, I will revisit this topic later. After a longer trial period I should be able to say something more conclusive.
Though I can't say anything especially positive (or negative, for that matter) about creatine on the physical front, I can say that I've felt positive effects mentally. I actually do feel more sharp and alert when I take it. As a result, I intend to extend the trial period I'm now undergoing and will probably be on creatine for at least the next three months or so. Again, I will post more information about its effects in the mental realm as I progress through this trial.
Relatedly, since, as I posted earlier, my blood pressure medicine (hydrochlorothiazide or HZ) would conflict with the creatine, I've stopped taking the HZ again (last dose taken on 1/6). This, in turn, has led me to be more conscientious about doing my breathing exercises. And I have to say that, most of these days I've not felt any high blood pressure indications--that is until today. I'm hoping I can attribute today's symptoms to the fact that, owing to some obligations that took up much of the day yesterday, I did not do my breathing exercises yesterday. I continue to hope that being very regular about these exercises is going to allow me to stay off the HZ and on the creatine.
On the breathing exercise front I do continue to feel immediate benefit from these. Just a little while ago I thought I felt a blood-pressure-related-headache coming on, but now that I've done my second set of breathing exercises for the day, the nascent headache seems to have dissipated. I'll certainly be posting more in the future about this.
For the record, I'm trying to do these breathing exercises twice a day--in the morning and right before bed--for about 10 to 15 minutes at a time. My breath-per-minute (BrPM) count continues to be lower than what's recommended--at about 4 BrPM--but I'm not doing any special straining to attain that, so I have to assume what I'm doing is safe.** My working hypothesis is that the recommended BrPM is higher than mine because most people with blood pressure problems are in much worse physical condition than me.
And, finally, we've started our interval training on the stationary bikes. I have to say that I really like this form of off-season training--it really offers a great way to mix things up in our fitness regimen. And, if certain studies are to be believed, doing intervals will allow us to keep in a form at least as good as what we'd get from a pure cardio stationary-bike routine while putting in less time.
I've modified things a bit from the regime the researchers used in the article I posted about (Fitness 'takes 6 minutes a week') some time ago and that touted the benefits of this type of training. The participants in that study used a pattern consisting of a 30-second burst followed by 4 minutes of leisurely riding over a 15 minute period. But I've found that I feel fully recovered after only about 2 minutes of leisurely riding following the 30-minute burst. So I've cut down the leisurely riding period to 3 minutes. I also feel that 15 minutes total time on the stationary bike is just too short so I'll increase it a bit. I'll be putting in between 20 and 30 minutes when doing this interval training over the remainder of the cycling off-season.
So the current routine is 4 times per week (Sat., Sun., Tues., Thurs.) stationary bike interval training and twice a week (Mon., Fri.) strength training. We now do our modified Power 90 routines for strength training, but we will soon move to a different routine for our twice-weekly strength-training sessions--at least up until cycling season begins in earnest.
Thanks for reading.
---------------------
* Ok, I know it's recommended to take 20 grams a day during this initial "loading" phase. But I'm trying to make the small quantity of creatine I bought for an initial test last until the next credit card billing cycle when I can buy some more. So I've made some dosage adjustments.
** I've read information indicating that the ideal BrPM is 5 to 6. Below 4.5 is said to be too low.
First thing to report on is creatine. I decided to just buy a small quantity and try it out for awhile. As you will be aware if you read my previous post, I'm hoping as much for a mental benefit from this as I for physical benefits.
Here's how it's going so far. I decided after doing some reading on the topic that, initially, I should take a larger dose of the creatine. So, for the first week--which will end this coming Thursday--I'm taking ca. 15 grams a day.* After that I'll cut down to the more normal daily dosage of about 5 grams daily.
We've only done one strength-training workout since I started this and I would say that so far I've noticed zero effect from the creatine so far as endurance or recovery are concerned. It's too early to say definitively whether it will have much effect in those areas but I can at least say that the initial impression I have is that it's unlikely to have any dramatic effect. That said, I will revisit this topic later. After a longer trial period I should be able to say something more conclusive.
Though I can't say anything especially positive (or negative, for that matter) about creatine on the physical front, I can say that I've felt positive effects mentally. I actually do feel more sharp and alert when I take it. As a result, I intend to extend the trial period I'm now undergoing and will probably be on creatine for at least the next three months or so. Again, I will post more information about its effects in the mental realm as I progress through this trial.
Relatedly, since, as I posted earlier, my blood pressure medicine (hydrochlorothiazide or HZ) would conflict with the creatine, I've stopped taking the HZ again (last dose taken on 1/6). This, in turn, has led me to be more conscientious about doing my breathing exercises. And I have to say that, most of these days I've not felt any high blood pressure indications--that is until today. I'm hoping I can attribute today's symptoms to the fact that, owing to some obligations that took up much of the day yesterday, I did not do my breathing exercises yesterday. I continue to hope that being very regular about these exercises is going to allow me to stay off the HZ and on the creatine.
On the breathing exercise front I do continue to feel immediate benefit from these. Just a little while ago I thought I felt a blood-pressure-related-headache coming on, but now that I've done my second set of breathing exercises for the day, the nascent headache seems to have dissipated. I'll certainly be posting more in the future about this.
For the record, I'm trying to do these breathing exercises twice a day--in the morning and right before bed--for about 10 to 15 minutes at a time. My breath-per-minute (BrPM) count continues to be lower than what's recommended--at about 4 BrPM--but I'm not doing any special straining to attain that, so I have to assume what I'm doing is safe.** My working hypothesis is that the recommended BrPM is higher than mine because most people with blood pressure problems are in much worse physical condition than me.
And, finally, we've started our interval training on the stationary bikes. I have to say that I really like this form of off-season training--it really offers a great way to mix things up in our fitness regimen. And, if certain studies are to be believed, doing intervals will allow us to keep in a form at least as good as what we'd get from a pure cardio stationary-bike routine while putting in less time.
I've modified things a bit from the regime the researchers used in the article I posted about (Fitness 'takes 6 minutes a week') some time ago and that touted the benefits of this type of training. The participants in that study used a pattern consisting of a 30-second burst followed by 4 minutes of leisurely riding over a 15 minute period. But I've found that I feel fully recovered after only about 2 minutes of leisurely riding following the 30-minute burst. So I've cut down the leisurely riding period to 3 minutes. I also feel that 15 minutes total time on the stationary bike is just too short so I'll increase it a bit. I'll be putting in between 20 and 30 minutes when doing this interval training over the remainder of the cycling off-season.
So the current routine is 4 times per week (Sat., Sun., Tues., Thurs.) stationary bike interval training and twice a week (Mon., Fri.) strength training. We now do our modified Power 90 routines for strength training, but we will soon move to a different routine for our twice-weekly strength-training sessions--at least up until cycling season begins in earnest.
Thanks for reading.
---------------------
* Ok, I know it's recommended to take 20 grams a day during this initial "loading" phase. But I'm trying to make the small quantity of creatine I bought for an initial test last until the next credit card billing cycle when I can buy some more. So I've made some dosage adjustments.
** I've read information indicating that the ideal BrPM is 5 to 6. Below 4.5 is said to be too low.
Labels:
blood pressure,
BrPM,
creatine,
hydrochlorothiazide,
intervals
Wednesday, January 6, 2010
Creatine?
I generally do not like the idea of dietary supplements, preferring to do things the natural way. But since I've noticed the term creatine bandied about a lot in fitness circles, I decided to look into it a little to see just what this is and what it does.
Well, the more I read about it, the more I began to think that this is something I should work into my dietary intake. It's used by many for muscle building, increasing endurance, and perhaps speeding recovery--the latter two of which I have no opposition to. But it is actually not primarily those uses that have got me thinking seriously about trying it.
Rather, what makes me think more seriously about it is that, in addition to those things, it is said to be of special benefit to vegetarians. And I happen to have been following a vegetarian diet for over 20 years.
It seems that creatine is a naturally occurring substance in the body, but also one that our bodies can absorb from certain foods--fresh meat being one of the main ones, it is said. Vegetarians, understandably, tend to be deficient in this substance. And one of the positive effects studies have shown creatine to have on vegetarians is to enhance mental performance (study cited in this Wikipedia article). I'm not sure why a lack of creatine would degrade mental faculties but, hey, at my age, I can use all the help I can get in heightening cognitive abilities.
So, what are the downsides? Unfortunately, there are some for me. While creatine seems a fairly safe supplement to use, it is said not to interact well with a medication I've recently had to resume taking--hydrochlorothiazide (HZ hereafter). See the National Library of Medicine page regarding creatine, where they recommend against combining it with HZ and other diuretics, here.
I'm excited to learn about creatine and its possible benefits for me. But at the same time I'm in kind of a quandary about what to do since I seem to need the HZ recently. I got a bit lax about my breathing exercises lately, though I've gotten more regular about them over the last few days (incidentally I've been consistently at around 4 BrPM and even saw 3.6 BrPM today with a little straining toward the end). Maybe by sticking more regularly with those exercises I can bring the blood pressure under control non-medicinally like I'd been hoping? That sounds like the way to go. At the moment it seems to me creatine offers too many benefits to not try taking it.

Well, the more I read about it, the more I began to think that this is something I should work into my dietary intake. It's used by many for muscle building, increasing endurance, and perhaps speeding recovery--the latter two of which I have no opposition to. But it is actually not primarily those uses that have got me thinking seriously about trying it.
Rather, what makes me think more seriously about it is that, in addition to those things, it is said to be of special benefit to vegetarians. And I happen to have been following a vegetarian diet for over 20 years.
It seems that creatine is a naturally occurring substance in the body, but also one that our bodies can absorb from certain foods--fresh meat being one of the main ones, it is said. Vegetarians, understandably, tend to be deficient in this substance. And one of the positive effects studies have shown creatine to have on vegetarians is to enhance mental performance (study cited in this Wikipedia article). I'm not sure why a lack of creatine would degrade mental faculties but, hey, at my age, I can use all the help I can get in heightening cognitive abilities.
So, what are the downsides? Unfortunately, there are some for me. While creatine seems a fairly safe supplement to use, it is said not to interact well with a medication I've recently had to resume taking--hydrochlorothiazide (HZ hereafter). See the National Library of Medicine page regarding creatine, where they recommend against combining it with HZ and other diuretics, here.
I'm excited to learn about creatine and its possible benefits for me. But at the same time I'm in kind of a quandary about what to do since I seem to need the HZ recently. I got a bit lax about my breathing exercises lately, though I've gotten more regular about them over the last few days (incidentally I've been consistently at around 4 BrPM and even saw 3.6 BrPM today with a little straining toward the end). Maybe by sticking more regularly with those exercises I can bring the blood pressure under control non-medicinally like I'd been hoping? That sounds like the way to go. At the moment it seems to me creatine offers too many benefits to not try taking it.

Saturday, January 2, 2010
The article from the future (on hormone replacement therapy)
The article doesn't really belong here. As you'll note, it was published in the New York Times something like two weeks after the date you'll see in the heading of this blog entry. Thanks to the magic of technology though, I can overcome barriers of time . . . sort of. Actually, I placed the article here because I'll want to refer to it later, but I didn't want it to interfere with the flow of my current (ca. 1/27/10) entries.
As you'll see, it's related to fitness and aging. The new approach, it seems, is to try and manipulate the aging organism pharmaceutically so as to stave off decrepitude and increase quality of life into middle age and beyond. I don't plan on trying something like this myself, preferring, instead, to maintain health the natural way. But since it concerns topics I write about in this blog I need to acknowledge its existence and address it in some way. Thus, the current "futuristic" entry.
As you'll see, it's related to fitness and aging. The new approach, it seems, is to try and manipulate the aging organism pharmaceutically so as to stave off decrepitude and increase quality of life into middle age and beyond. I don't plan on trying something like this myself, preferring, instead, to maintain health the natural way. But since it concerns topics I write about in this blog I need to acknowledge its existence and address it in some way. Thus, the current "futuristic" entry.
January 17, 2010
Vigor Quest
By TOM DUNKEL
NEARLY EVERY SUNDAY morning — Easter and Mother’s Day included — John Bellizzi says goodbye to his wife, Francesca, grabs an equipment bag and slides into the front seat of his black BMW. He drives to a high-school soccer field about 10 miles from his home in the New York City suburb of Rye.
Bellizzi, who is 51, is a member of the Old Timers Soccer Club, a band of stubborn, aging athletes who refuse to fall under the spell of golf. Technically, these are just pickup games, but they have been happening weekly since the early 1980s. The players go to the trouble of hiring a referee and battle full tilt (think slide tackles and heels-over-head bicycle kicks) for an hour and a half. Many of them were high-school and collegiate stars, decades ago. “One guy had a hip replacement,” Bellizzi, a former soccer captain at Queens College, says. “He was out for a year, then he came back.”
Advil, hot tubs and surgery keep most of the Old Timers going, but Bellizzi has ventured further. Two summers ago he became a patient of Dr. Florence Comite, a Manhattan endocrinologist affiliated with Cenegenics Medical Institute. Cenegenics, a privately held company based in Las Vegas, claims to have 10,000 patients and annual revenue of $50 million, making it the country’s foremost purveyor of so-called age-management medicine.
Comite’s relationship to Bellizzi is like that of an ace mechanic to a classic car. Her job is to keep him finely tuned despite worn parts. “I consider what I do aggressive prevention, the basis of which is metabolism modulation,” Comite says. “Twenty years from now, this will be the standard of care.”
Bellizzi is a vice president of business development at Thomson Reuters. Every three months a Cenegenics contractor comes to his office in Stamford, Conn., and draws 10 vials of blood. Comite receives a lab report that isolates scores of variables on those samples, among them glucose and cortisol, a stress hormone produced by the adrenal glands. The readings, in part, tell her if any metabolism tweaking is in order.
Under Comite’s guidance — and at an annual cost of about $10,000, most of it not covered by insurance — Bellizzi has gobbled vitamins and prescription-strength Omega-3 fatty acids. He follows a low-glycemic diet, lifts weights and jogs, all of which is familiar-enough health-and-fitness fare. Comite asserts, however, that “lifestyle alone isn’t enough” to counter the corrosive effects of aging. Therefore, twice a week Bellizzi grabs a pinch of abdominal skin and injects himself with human chorionic gonadotropin, or H.C.G., a hormone distilled from the urine of pregnant women.
H.C.G. is commonly used as a fertility drug. Comite uses it for an alternative application that’s perfectly legal and, she insists, safe: regular doses of H.C.G. signal the testes to secrete more testosterone, which the body generates in progressively smaller amounts after about age 30.
Testosterone is a naturally produced anabolic steroid, best known as the male sex hormone. But Comite and a growing minority of physicians regard it as motor oil that keeps bodies running smoothly. For testosterone to trigger a cellular response, receptors must be present to receive its coded messages. Surprisingly, testosterone receptors are highly concentrated inside the heart, indicating its larger biochemical role. Numerous studies, Comite says, show that low testosterone contributes to a loss of lean muscle mass, bone density, energy and libido, thereby making older men more susceptible to cardiovascular disease, diabetes, osteoporosis, sexual dysfunction and, possibly, depression.
Comite says she believes in the existence of male menopause. She pegs it to when the testicles stop responding to a testosterone stimulant like H.C.G., for all intents and purposes shutting down. That occurs anywhere between the ages of 45 and 75. Women also produce testosterone, though in relatively small amounts. Female hormone production is prone to sharp spikes and dips, moving in concert with the fertility cycle. For males, fluctuations tend to be less extreme. Still, similarities between the sexes far outweigh any differences. Both men and women experience systemic changes associated with aging that “lead you down the path to disease,” Comite says.
Mainstream medicine does not join her in embracing the idea of male menopause. The position of the National Institute on Aging is that “there is scant scientific evidence that this condition, also known as andropause or viropause, exists.” Likewise, micromanaging the body’s metabolism strikes most physicians as an overly bold intervention: yet to be proved at best, dangerous at worst. The Endocrine Society, for example, questions the benefits of testosterone therapy except when administered to counteract a specific malady like delayed puberty or AIDS wasting. The society’s guidelines “recommend against . . . offering testosterone to all older men with low testosterone” barring definitive proof of its efficacy.
S. Jay Olshansky, a professor of public health at the University of Illinois at Chicago, is an author of “The Quest for Immortality: Science at the Frontiers of Aging” and is at work on a sequel titled “Huckster’s Paradise.” He is wary of most things that smack of antiaging medicine.
“If anyone is arguing that this is the new medical profession or the way things are going to be done 20 years from now, I would say they’re drinking the Kool-Aid of the antiaging industry,” Olshansky says. “They’re making money selling a repackaged version of traditional preventive medicine, and then they add some hormones and supplements. It’s just such a racket.”
Comite’s notion of metabolism modulation extends beyond H.C.G. and testosterone. It encompasses health-food-store staples like the fruit extract saw palmetto and vitamin D, as well as heavier artillery that includes melatonin (an antioxidant), dehydroepiandrosterone (the body’s most abundant steroid) and even human-growth hormone. When it comes to testosterone, she opts for injections over more user-friendly gels and patches.
Comite has impeccable credentials. After graduating from Yale School of Medicine and working at the National Institutes of Health in Bethesda, Md., she was a part-time faculty member at Yale, a job she has held for the last decade. Much of her recent professional life is devoted to bridging the divide between conventional medicine and age-management medicine. That bridge probably won’t be completed anytime soon. Do a Google search of “Florence Comite” and the first item that pops up is her biographical entry on the Web site Quackwatch.com.
John Bellizzi has unwavering trust in her, though. They talk for hours on end about body chemistry, his treatment and lab results. Comite has pored over generations of his family medical history and sent him multiple research studies.
“This notion of ‘we’re getting old; it’s bound to happen’ doesn’t make any sense to me,” Bellizzi says. “I don’t think I’m so far out on the edge here that I’m gambling with my life. What I do know is I feel better.”
It may be tempting to dismiss Bellizzi as a soccer fanatic afraid to age gracefully or to accuse Comite of squandering her talent by catering to affluent, youth-clinging patients. Nonetheless, their medical partnership could have broad, perhaps profound, implications. At root, this is a tale of empowerment, of humankind’s primordial urge to exert control over the aging process. That raises intriguing questions. What constitutes responsible cutting-edge science as opposed to a reckless pushing of the envelope? Where is the line separating a vanity fix from a genuine quality-of-life improvement? Imagine that a miracle drug is discovered that guarantees vigor far beyond retirement age, but shortens your life by, say, four years. Is it worth the trade-off?
The human body is a symphonic masterpiece of flesh and blood, but it wears out like any clanking machine on the factory floor. The ruthless tick, tick, tick of time strips gears, nibbles at bushings. On a submicroscopic level, damage is done by free radicals, unstable atoms that have a toxic effect on cell membranes and DNA. In addition, telomeres, the protective tips on chromosomes, fray from the stress of continual regeneration, much as serial photocopies of an image lose their crispness.
Some antiaging proponents make seductive promises about prolonging longevity. Comite steers clear of that camp. Her interest lies in extending the length of “health span,” as opposed to life span. Does the body have to slide inexorably downhill after 40? She says she is convinced that metabolism modulation can help stave off stroke, heart disease and diabetes; can flatten the trajectory of corporeal decline. Ideally, age-management-medicine patients will keep humming along nicely, then crash like a spent computer. As Comite puts it, “Can we maintain optimal health until one day when we just don’t wake up?”
Tantalizing though it is, Comite’s question is just philosophical conjecture. But the first hint that such a situation might be achievable came in a study that appeared in the July 5, 1990, issue of The New England Journal of Medicine. Dr. Daniel Rudman wanted to test the prevailing notion that older people lose muscle and gain fat because they produce less growth hormone. Twelve men, ages 61 to 81, were given small doses of synthetic human-growth hormone three times a week. After six months they showed a 9 percent increase in lean-muscle mass, a 14 percent decline in fat and a modest improvement in bone density. “The overall deterioration of the body that comes with growing old is not inevitable,” Rudman declared. “We now realize some aspects of it can be prevented or reversed.”
Rudman, who has since died, reportedly came to regret his choice of words and the fact that so many overlooked that this was a small test-group participating in a short-term study; it was not an experiment he intended to be conclusive. Still, a kind of growth-hormone and anabolic-steroid gold rush ensued — witness the fact that today you can buy hormones from China online and consult how-to books like “The Secrets of Mail Order Steroid Success.”
Within two years of Rudman’s study, the American Academy of Anti-Aging Medicine was established. It unabashedly presses the case for growth hormones, but there’s room in the tent for low-level light therapy, whole-body vibration machines and assorted New Age nostrums. The organization boasts of being “the first scientific nonprofit medical society to forecast the deliverance of human life spans in excess of 100 years.” A Chicago-area doctor and amateur bodybuilder named Alan Mintz also took keen interest in Rudman’s experiment. Mintz was soon augmenting his gym workouts with testosterone and growth hormone. He and his exercise partner, John Adams, owned a radiology-diagnostics company. They sold the business in 1994, pocketing millions. Rather than retire and work full time on their pecs, they started Cenegenics Medical Institute, a boutique age-management center, and relocated to Las Vegas.
The cultural demographics couldn’t be better for their company. Baby boomers — some 79 million strong — are going gray. Many, like John Bellizzi, refuse to surrender their youth without a fight. By the summer of 2008, he was closing in on 50: pudgy, sluggish and worried he had lost his edge at work as well as on the soccer field.
Flipping through an airline magazine while on a business trip, Bellizzi stumbled on an ad for Cenegenics Medical Institute. It featured startling photographs of Dr. Jeffry Life, a Cenegenics physician. The “before” shot showed Life with a pot belly and noodle arms. The “after” picture looked like some grandfather’s head had been superimposed on Mr. Universe’s body. Apparently no trick photography was involved; that was Life showing off his new age-management-medicine physique.
Bellizzi pondered the ad for a few months, then called Cenegenics’ toll-free number. Soon he was sitting in Comite’s office on East 86th Street, exhibiting classic signs of the middle-age fade. Blood tests showed he had an underactive thyroid. He was flirting with obesity. He had high cholesterol and low testosterone. Comite made immediate diet and exercise suggestions and put him on thyroid medication; then six months later she prescribed the H.C.G. booster. She opted for using H.C.G. because it nudges the testicles into making more testosterone. With direct testosterone injections, they would be bypassed entirely and gradually atrophy.
Bellizzi used to collapse exhausted on his couch after soccer games. Now, he says, he can “play for another hour.” He feels mentally sharper and is 15 pounds lighter. It’s difficult to say what’s benefiting him most. Eating more protein or laying off the Häagen-Dazs ice cream? Running four times a week? Bellizzi says he thinks H.C.G. deserves a great deal of credit too, while acknowledging it is “fairly controversial.”
Consensus is elusive in the realm of age-management medicine. There are known side effects for the more controversial treatments. For growth hormone: joint pain, fluid retention, a possible diabetes link; for testosterone: thickening of the blood, rashes, swelling of the breasts. There is a strong presumption that those compounds will supercharge an existing cancer. Some doctors, however, say these effects can be controlled or eliminated by monitoring dosages and screening at-risk patients.
But the bigger issue is that the medical literature pertaining to steroids and hormones is characterized by a dearth of long-duration, large-population, placebo-controlled studies. “The same body of data, different people look at it and have very strong and opposing points of view,” says Dr. Shalender Bhasin, a professor at Boston University School of Medicine and chairman of the Endocrine Society’s testosterone-guideline panel.
The Food and Drug Administration originally approved human-growth hormone as a treatment for stunted growth in children and then for atrophy in AIDS patients, but later authorized it for what is termed “adult growth-hormone deficiency.” There is wiggle room as far as interpreting that syndrome and therefore opportunity for unscrupulous doctors to prescribe the drug for somebody who merely wants to bulk up and look buff.
Dr. Tom Perls, an associate professor of medicine also at Boston University School of Medicine, has testified before Congress that growth-hormone deficiency occurs only in about 1 adult out of 10,000. By comparison, nearly 10 percent of Cenegenics’ patients receive human-growth hormone. Perls says he believes some age-management doctors fudge their diagnoses. “They certainly could be well meaning,” he says, “but I think it’s irresponsible to treat people, particularly with potent drugs, just because you yourself think it has some benefits.”
Critics cite situations in which physicians enthusiastically prescribed Vioxx with disastrous consequences or prescribed hormones for postmenopausal women only to learn about an N.I.H. study released later that linked those hormones to breast cancer. They cite the case of the professional wrestler Chris Benoit, who regularly injected freakishly high amounts of testosterone and who committed suicide after killing his wife and son. Then there’s Hanneke Hops, a 56-year-old Californian who died of liver cancer in 2004, six months after becoming a Cenegenics patient. Her family says growth-hormone supplements aggravated latent tumors. Alan Mintz called that “speculation,” saying his company would never give hormones to anyone suspected of having cancer.
Advocates of age management have their favorite rebuttals. If athletes abused insulin, nobody would seriously consider outlawing it for the treatment of diabetes, they say. We don’t accept osteoporosis as a necessary condition of growing old. Why not be just as proactive with declining hormones as we are with brittle bones?
Dr. Marc Blackman is associate chief of staff for research and development at the Veterans Affairs Medical Center in Washington. Regardless of the quality and quantity of cumulative human research, many holes remain, he says. What constitutes low testosterone for a man at age 40? At 60? At 80? Thus far, there are no universal standards. Blackman, an endocrinologist, poses a cogent question: “How do you distinguish between a normal age decline and a chemical deficiency?”
That’s “the art” of medicine, Florence Comite says. Judgment calls have to be made. She worries more about what gets lost in this discussion; namely, the wide-angle view of her kind of intense preventive medicine. True, her methods are expensive. But she imagines an affordable model designed for the masses, one that would be an antidote for what’s ailing America’s disease-based health care system. “This isn’t about the future Fountain of Youth,” she says. “This is about the big picture.”
COMITE GREW UP in Brooklyn and Queens, a daughter of Holocaust survivors. Family members were so hungry for knowledge that they read not only at the dinner table but also while washing dishes. Her favorite book as a teenager was “Stranger in a Strange Land,” Robert Heinlein’s science-fiction classic about an earthling boy raised by Martians. Like the book’s hero, Comite knew something about alien environments. She graduated from high school at 16, sped through Brooklyn College and entered Yale Medical School at 20. Next came a fellowship in reproductive endocrinology at the National Institute of Child Health and Human Development, which led to a job at N.I.H. doing research in gynecology and precocious puberty.
In 1985, Comite returned to Yale as part of the medical faculty. In addition to teaching, she founded Women’s Health at Yale, arguably the first clinic in the country to treat women’s health issues as a special discipline. Many men on the faculty questioned the need for such a clinic. Comite says she used to “wake up scared” at night, career-killer thoughts racing through her head. What if I’m wrong? What if I’m going down a path that doesn’t lead anywhere?
“It was not a hot topic, and medicine in general was not interested in women’s health,” Dr. Paul Barash, a professor of anesthesiology at Yale, says. “ ‘Eclectic’ is a very good term to describe her. Basically, she had to mobilize public opinion to start getting women’s health on the radar screen.”
Comite left a tenure-track position at Yale because she became frustrated with what she saw as medicine’s red tape and tunnel vision. One galvanizing moment involved a woman named Vivian, who had a badly scarred uterus and who had tried repeated in vitro fertilizations without success. She came to see Comite at Yale, still hoping to have a child, but failed to conceive. At wit’s end, Vivian consulted an acupuncturist. She became pregnant after only a few treatments.
“I would swear on a stack of Bibles and all my oaths there was no way that woman could conceive,” Comite says. “That experience turned me into an open-minded skeptic.”
This ushered in a restless phase of her career. Comite briefly reconnected with the N.I.H. as a research adviser. She helped establish a women’s health clinic in Egypt, served on an Institute of Medicine committee that compiled a report on alternative medicine. Comite went into private practice in January 2005, doing what she does now but not articulating it as age-management medicine per se. That June, Alan Mintz invited her to Las Vegas, and she ultimately joined Cenegenics’ medical advisory board. (Two years later, Mintz, while doing an overhead press in the gym, lost control of the weighted bar, which struck him in the back of his head. He died while undergoing a brain biopsy.)
About 80 percent of Comite’s patients are men. It’s a good match. She finds male menopause an area ripe for exploration, and men are generally more receptive to the notion of age management than women, who have been bombarded for years with conflicting information about hormone therapy.
Bob Fitzmaurice, a 48-year-old New Hampshire businessman, spent seven years trampolining around to doctors and psychiatrists, searching for relief from a crippling lethargy. Comite treated him for abnormally low testosterone. Jerome Baron, 83, made an appointment at the behest of his son, who was already a Comite patient. He had fallen several times, once breaking his nose. He takes a shot of testosterone every week and about 45 vitamins and nutrition pills every day. “I don’t trip,” Baron cheerfully remarks. “I’m stronger. My legs are stronger.” And there’s an added bonus: “I started to get urges for sex, which I hadn’t had in a few years.”
Critics scoff at such anecdotal evidence. Comite understands that it comes with the territory. One of the lessons Yale taught her is that change makes most people “uncomfortable.” A vignette sticks in her mind. She was a junior faculty member, walking down a corridor one afternoon at the medical school, when a distinguished department head sidled up to her. She says he icily remarked, “The problem with you, Florence, is that you’re an independent thinker.” That was not meant to be a compliment. She considers it one of the nicest things anybody has ever said to her.
THE HEADQUARTERS OF Cenegenics Medical Institute sits on the fringe of Las Vegas, where the pavement peters out and turns to desert sand. The facade of the two-story building, with its picket line of alabaster Corinthian columns, evokes a Greek temple. This could be an embassy in some sun-drenched principality: the People’s Republic of Rejuvenation.
Dr. Jeffry Life, dressed in a dark suit and with a Bluetooth headset clinging to one ear, was seated at a desk inside a cramped, temporary office. He was in the process of moving off campus. His Cenegenics ads succeeded beyond his wildest expectations, becoming the focal point of a $5 million a year media blitz. Life had decided to lighten his Cenegenics load in favor of pursuing spinoff opportunities: speaking engagements, a book deal, a Web site and a wellness center in Las Vegas under the Cenegenics banner.
“I want to get my message out to a wider audience,” he said, his voice simultaneously authoritative and avuncular. “I want to capitalize on this image I’ve created.”
Life’s message is that if a fat, 59-year-old, divorced family physician from eastern Pennsylvania can reinvent himself through a combination of lifestyle alterations and modern pharmacology, so can you. (By the way, that makeover didn’t include his name. He was born Jeffry Life.) In June 2003, Life signed up as a patient with Cenegenics and a year later joined the corporate team, which now includes 40 staff physicians in Las Vegas and in branches in eight other cities, with five more scheduled to open soon.
Every year, Life gets a new set of beefcake photos taken. Now 71, he said he put on five pounds of muscle this past year by scheduling extra tae kwon do practices and cranking it up a notch in the weight room. He can bench-press 235 pounds and can do 10 pull-ups, “full extension.”
His age-management program could fill a spreadsheet. Life began reciting from memory: 1,000 milligrams of calcium daily, coenzyme Q10 pills twice a day, 5,000 units of vitamin D, 4 grams of fish oil, 10 milligrams of melatonin at bedtime, a testosterone injection once a week, human-growth hormone once a day. “That reminds me,” he said, reaching into his desk drawer. “I’ve got to give myself a shot.”
He pulled out a syringe, loaded up on human-growth hormone, raised a pants leg and stuck the needle into his left thigh.
Life is good for Dr. Life. He relocated, remarried and rediscovered what it feels like to be 30. “I sometimes think what would have happened if I’d started this at 45 like a lot of my patients,” he mused.
Doctors and their family members account for about a quarter of Cenegenics’ patients, according to John Adams, the company president. Roughly 75 percent of them are men, and the recession doesn’t appear to be discouraging newcomers. Cenegenics’ revenue rose 35 percent in both 2007 and 2008, and growth was 10 percent in 2009, Adams said. There’s a five-month waiting list for doctors wanting to enroll in one of Cenegenics’ training seminars, but professional suspicion lingers. A neonatologist in Florida recently became a Cenegenics patient, but didn’t tell any of his physician friends. “They would think I’m crazy or vain or stupid,” he says.
Dr. Pinchas Cohen, chief of endocrinology at Mattel Children’s Hospital U.C.L.A. and a member of the Growth Hormone Society’s executive board, concedes that Jeffry Life “looks pretty good” but cautions that he is flirting with disaster because of the possible deleterious effects of human-growth hormone and testosterone: “I’m quite sure that he will end up a tragic case. Sooner or later, his cancer or diabetes will be diagnosed.”
Every field of medicine is in constant flux. Old maxims evolve into newer truths; yesterday’s hypothesis becomes tomorrow’s scientific breakthrough or dead-end fizzle. But that process of intellectual friction can generate a lot of emotional heat.
“There is a fascinating but very clear philosophical divide between the antiaging folks and mainstream medicine,” says Dr. Abraham Morgentaler, associate clinical professor of urology at Harvard Medical School. “What’s remarkable to me is how everybody has an opinion that often isn’t based on much.”
Morgentaler has no ties to Cenegenics Medical Institute. The feuding over testosterone therapy in particular piqued his curiosity. When he was in medical school, the accepted truth was that the higher a man’s testosterone level, the greater his risk of contracting prostate cancer. Morgentaler decided to investigate that premise, unearthing as many related research papers as he could, dating back more than half a century. The trail led him to a study done in 1941 that helped Dr. Charles Huggins win a Nobel Prize. Huggins’s focus was advanced prostate cancer. He discovered testosterone can feed existing tumors, a revelation that has stood the test of time. But other studies extrapolated on Huggins’s work, Morgentaler says, sparking a chain reaction of soft science that went a step further and implied that testosterone causes prostate cancer. As Morgentaler delved deeper, he said he was “dumbfounded” at all the positive evidence of testosterone’s general health benefits that had been ignored. His research odyssey turned into a book, “Testosterone for Life.”
“The stuff Dr. Comite is talking about is real,” says Morgentaler, referring to the biological causes of middle-age malaise. He frequently prescribes testosterone and offers this prediction: within five years testosterone will be as popular a yardstick of good health as cholesterol. “There are all these people walking around the United States who are getting older,” he said. “They know they don’t feel right. They’ve lost pep. Their brain doesn’t work as well. Mainstream medicine has no answers for them.”
ON A FEBRUARY afternoon seven and a half months into his Cenegenics journey, John Bellizzi sat on a stationary bicycle in Comite’s Manhattan office, pedaling as if he were on a Tour de France hill climb. He was in the final stages of a VO2 aerobic fitness test. A conelike rubber mask covered his nose and mouth, sucking up information from his labored breathing. Lance Armstrong pedals a test bike like this for an hour at high resistance. Bellizzi cranked for 12 minutes. “I couldn’t have done a lot more,” he said upon dismounting.
Steven Villagomez, an exercise physiologist, stood close by. “I’ll go over this with Dr. Comite,” he said, scanning a computer printout. “She’ll be thrilled to see these numbers.”
Since his intake exam in June 2008, Bellizzi had seen his weight drop to 165 pounds from 181; body fat to 15 percent from 27 percent. His cholesterol level declined to 162 from 231 and continues to fall.
“Your heart is stronger, pumping more effectively,” Comite pronounced after digesting his VO2 results. This summer Bellizzi celebrated his first anniversary of treatment. He’s feeling energetic enough that Comite has twice cut his H.C.G. dosage. His body is generating double the amount of testosterone that it did a year ago.
Is this the future of health care? Will metabolism modulating soon gain widespread acceptance? The National Institutes of Health announced in November that they are embarking on a six-year, $45 million study of the mental and physical benefits of testosterone therapy. Eight hundred elderly men will undergo tests at 12 facilities nationwide.
Preliminary results of the Testosterone Trial, as it is called, won’t be available until at least 2015. In the meantime, Bellizzi’s one-man experiment rolls on. He and his wife weighed the pros and cons over a kitchen-table brunch of fresh fruit and organic yogurt following a Sunday soccer game.
“I wish he wouldn’t do it,” Francesca said. She’s comfortable with everything but the H.C.G. injections. Have they done enough testing? Is this worth the expense and the uncertainty?
“I’d be a little concerned about taking testosterone,” John admitted. “I’d have to re-evaluate. But I’d be very leery about H.G.H. and doing more hormone modulation than I am now.”
The majority of Comite’s patients never need human-growth hormone, although a guy who says he intends to kick soccer balls until “the pain exceeds the pleasure” may want to keep that option open. As for testosterone, H.C.G. eventually loses its effectiveness as the testicles run dry. The only option is to turn to synthetic testosterone.
Comite has no doubt, when that time comes, that Bellizzi will make the decision to start injecting testosterone. “He’ll make it because he’ll realize he’s not feeling as good as he was before,” she says.
Maybe he will reach for the needle. Maybe he won’t. Right now, all Bellizzi knows is that he’ll be playing soccer next Sunday.
Subscribe to:
Posts (Atom)